Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: From the Human rights approach, dignity is accepted as a universal need, required for the well-being of every individual. It is an irrevocable feature of personhood that does not depend on or varies according to circumstances. However, in the medical context, what dignity entails in practice will also depend on patients´ perception of themselves, how others see them, and how the nature of the illness in question affects the person’s life and identity. It evokes the patient’s sense of autonomy and control. The loss of perceived dignity is an existential source of Human suffering rarely explored among patients with rheumatic diseases (RMDs), which contrasts with their observations that dignity, identity, and Quality of Life (QoL) are essential areas for research focus. We recently observed that distress related to perceived dignity (DPD) was present in 26.9% of Mexican outpatients with different RMDs.
The current study complements the research on the topic and investigates the factors associated with DPD in primary outpatients with different RMDs.
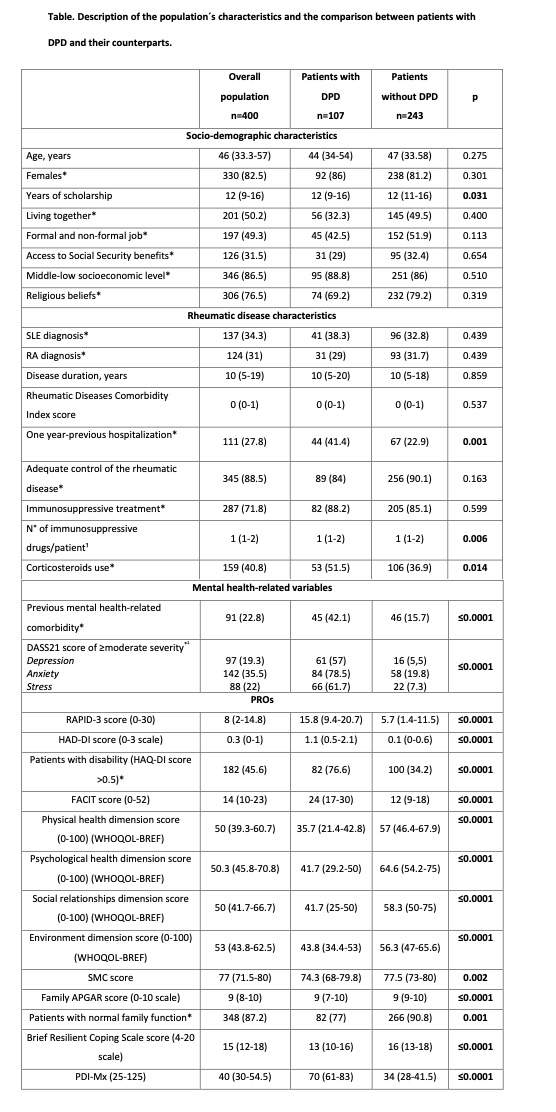
Methods: This cross-sectional study was performed in February-September 2022. Consecutive primarily outpatients with RMDs completed patient-reported outcomes (PROs) (to assess mental health [DASS-21], disease activity/severity [RAPID3], disability [HAQ-DI], fatigue [FACIT], QoL [WHOQOL-BREF], satisfaction with medical care [locally adapted questionnaire], resilience [brief-resilient coping scale] and family function [family APGAR]) and had a rheumatic evaluation to assess disease activity status and comorbidity (Rheumatic Disease Comorbidity Index). Sociodemographic variables and disease-related and treatment-related variables were retrieved with standardized formats. DPD was defined based on a score ≥ 54.5 (min 25-max 125) on the previously adapted and validated Mexican version of the Patient Dignity Inventory (PDI-Mx). Multivariate regression analysis was used to identify factors associated with DPD (the dependent variable). We estimated a sample size of 334 patients (considering 20% of losses for non-analyzable data) to achieve the objective described.
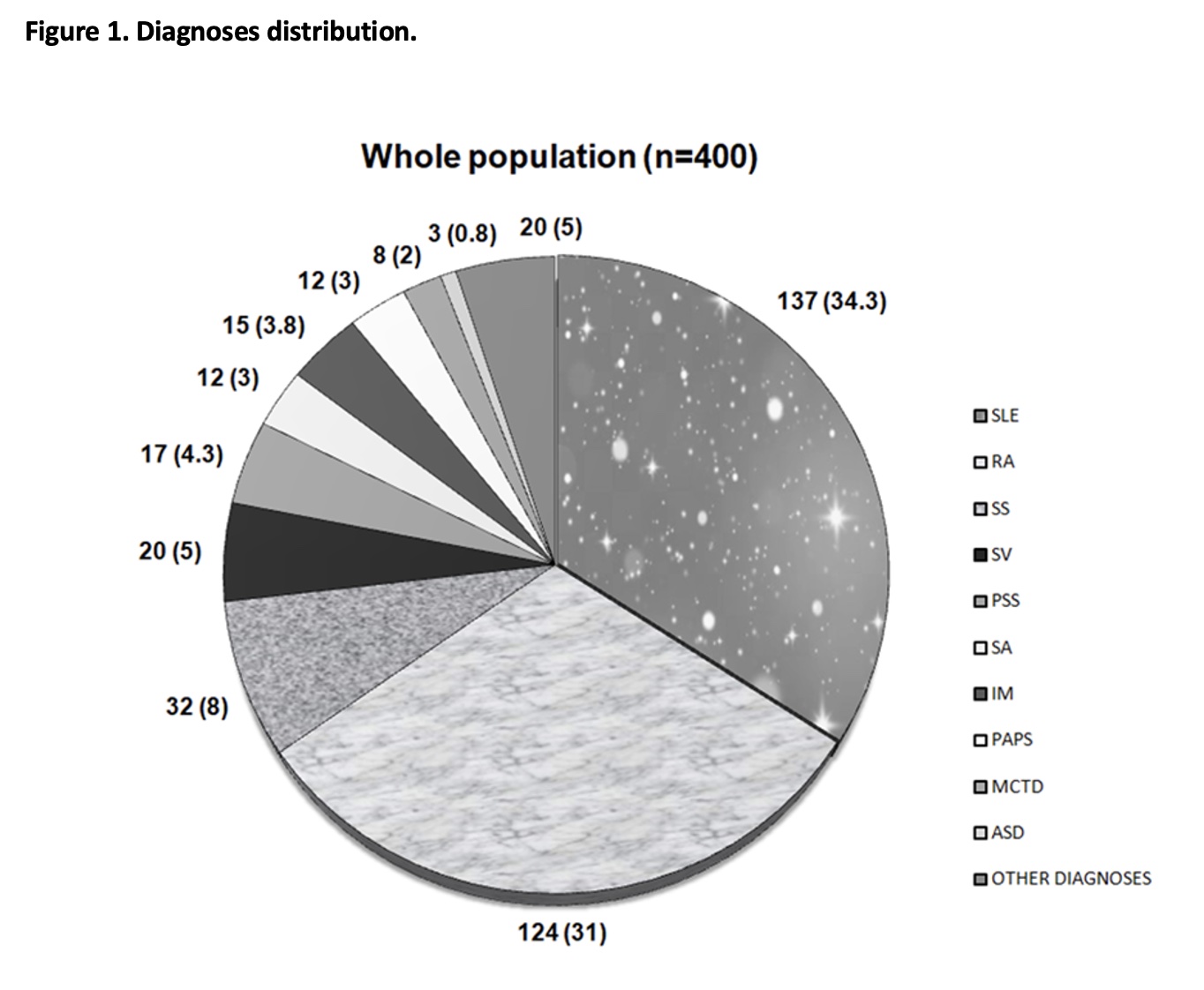
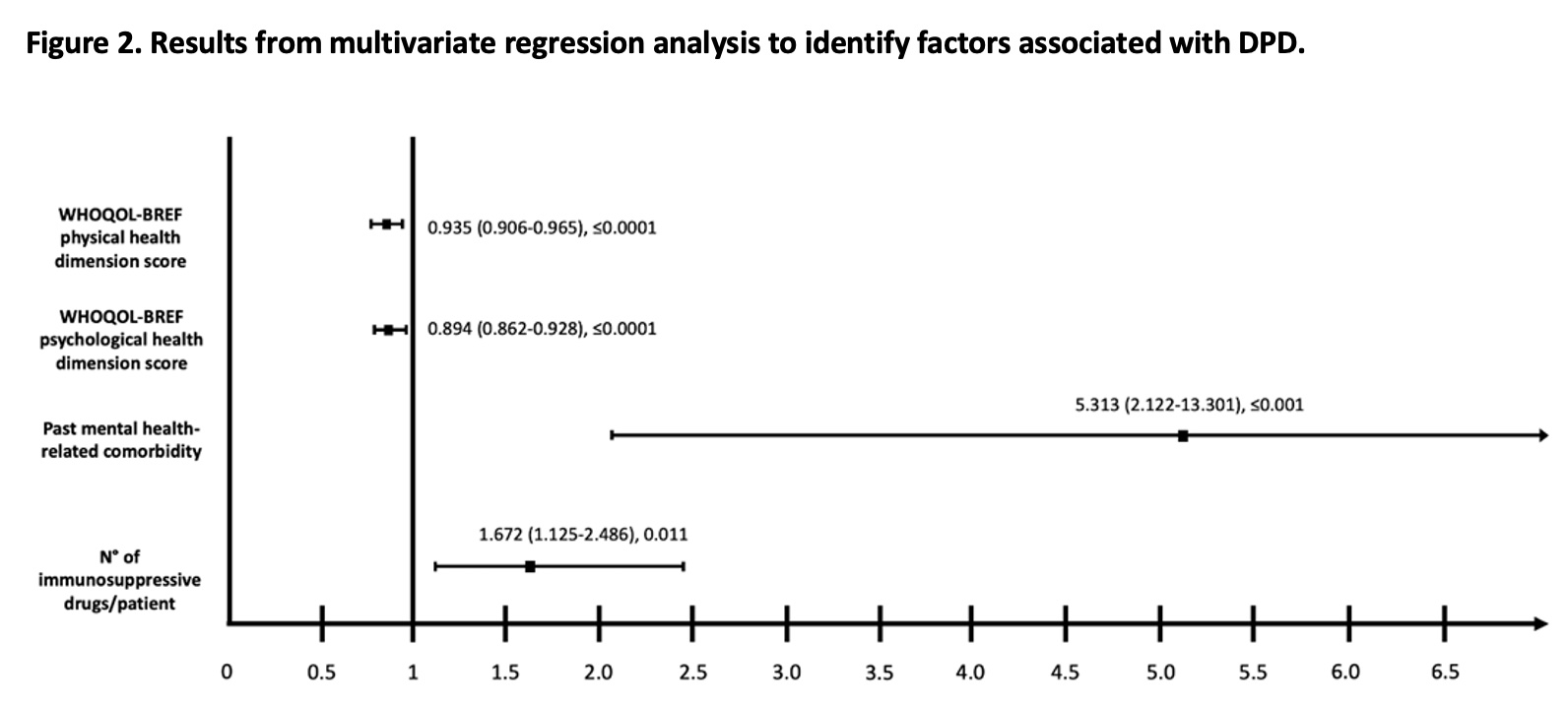
Results: Four hundred patients were included (February-September 2022), representing patients with RMDs and the most frequent rheumatic diagnoses in our outpatient clinic (Figure 1). One hundred and seven patients (26.8%) had DPD. They differed from their counterparts (less educated, with intensive treatment, mental health comorbidity, and worse PROMs) (Table). Past mental health-related comorbidity, the number of immunosuppressive drugs/patient, the physical health dimension score of the WHOLQOL-BREF, and the emotional health dimension score of the WHOLQOL-BREF were associated with DPD (Figure 2).
Conclusion: We observed that DRPD was present in a substantial proportion of patients with RMDs and was associated with previous mental health comorbidity, intensive treatment of the underlying RMD, and the patient QoL. Recognizing factors associated with DPD is an essential step in the right direction toward understanding the impact of RMDs in patients’ lives and preventing poorer prognoses.
To cite this abstract in AMA style:
Pascual Ramos V, Guaracha Basañez G, Contreras Yañez I, Cuevas Montoya M, García Alanís M, Rodríguez Mayoral O, Chochinov H. Factors Associated with Distress Related to Perceived Dignity in Patients with Rheumatic Diseases [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/factors-associated-with-distress-related-to-perceived-dignity-in-patients-with-rheumatic-diseases/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/factors-associated-with-distress-related-to-perceived-dignity-in-patients-with-rheumatic-diseases/