Session Information
Date: Tuesday, November 9, 2021
Title: Patient Outcomes, Preferences, & Attitudes Poster IV: COVID-19 (1589–1613)
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: COVID-19 vaccination is particularly important for patients with systemic rheumatic diseases (SRDs), who may be at increased risk of infection with SARS-CoV-2 and of worse COVID-19 outcomes. However, despite remarkable vaccine safety and efficacy data, some individuals remain hesitant to be vaccinated. We aimed to measure the degree of vaccine hesitancy in rheumatology outpatients from a U.S. COVID-19 “hotspot” and explore factors associated with hesitancy or refusal in this high-risk patient population.
Methods: We emailed a secure web-based survey on March 5, 2021 to 7,505 patients aged ≥18 years evaluated at least once by a rheumatologist between 2018-2020 at a large Rheumatology center in New York City and who previously agreed to participate in surveys on COVID-19. We included individuals who completed a modified vaccine hesitancy questionnaire (based on Larson et al. Vaccine. 2015), with questions specific to COVID-19 vaccination. We also collected data on sociodemographics, medical comorbidities, medication use, other immunizations during adulthood, and COVID-19 history. ICD-10-CM algorithms were used to identify SRD diagnoses. We evaluated patient characteristics and vaccine hesitancy questionnaire responses by vaccination status (refusing vaccination, undecided, already received/willing). Categorical variables were calculated using chi-square/Fishers exact test. Continuous variables were tested with one factor ANOVA.
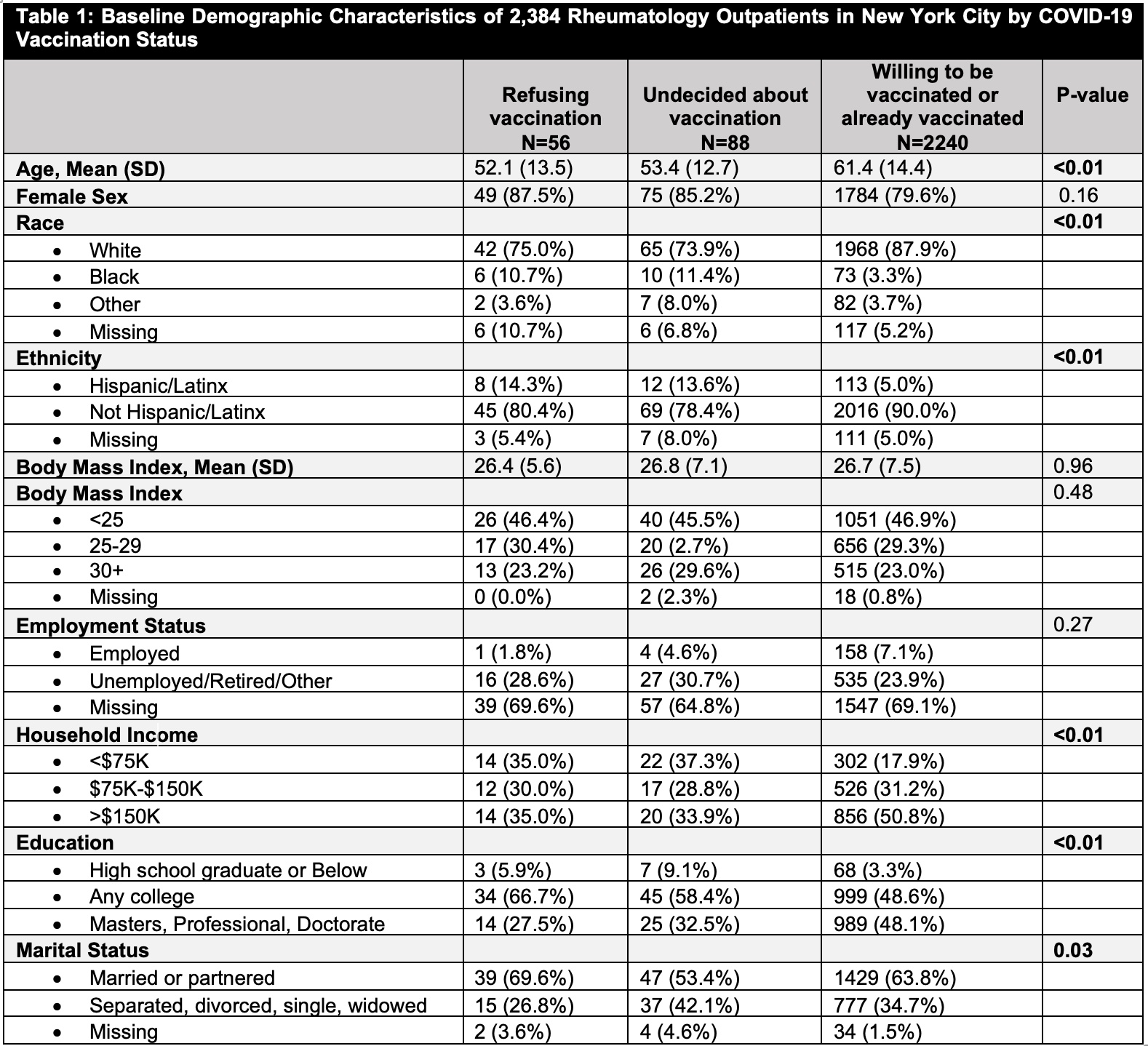
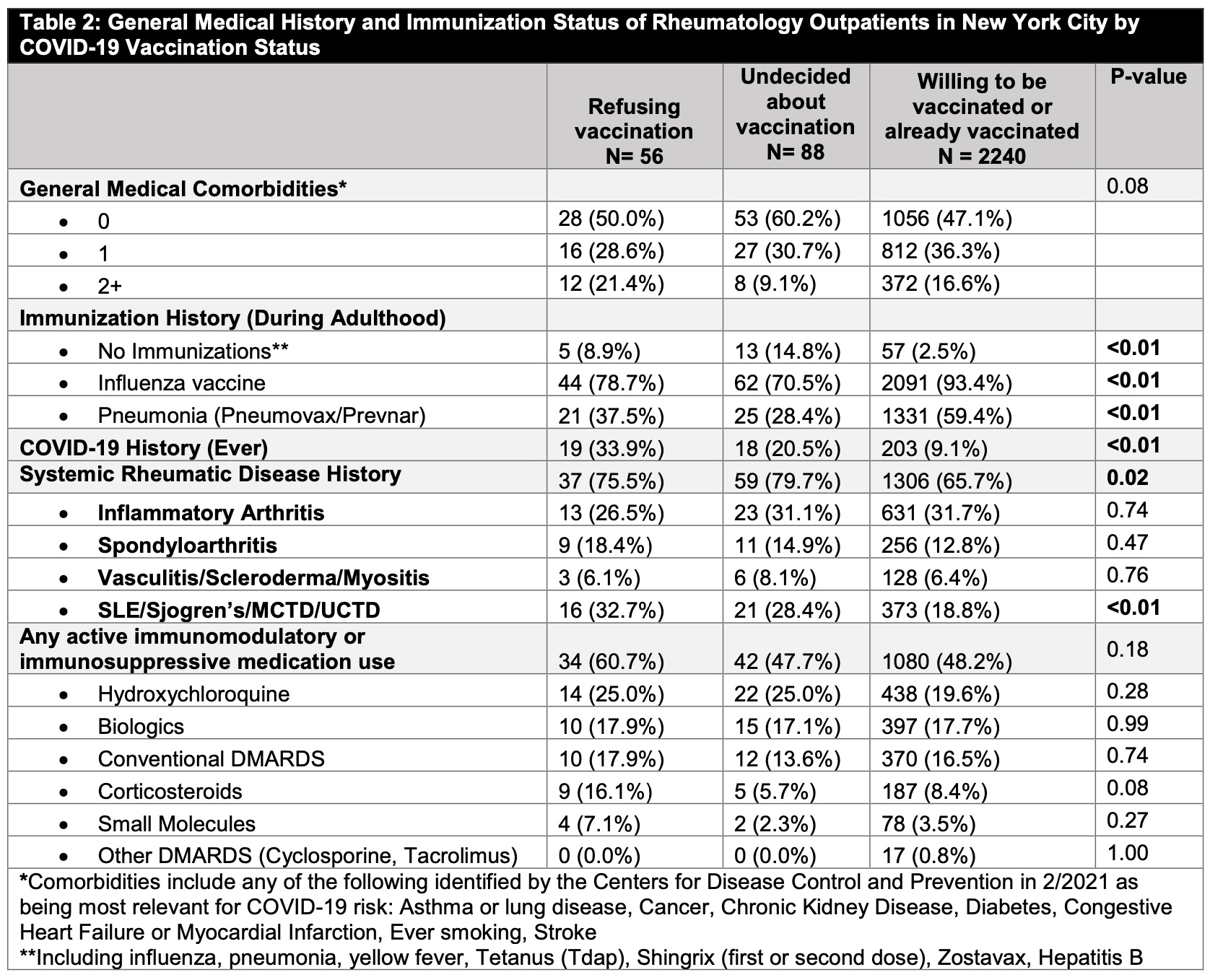
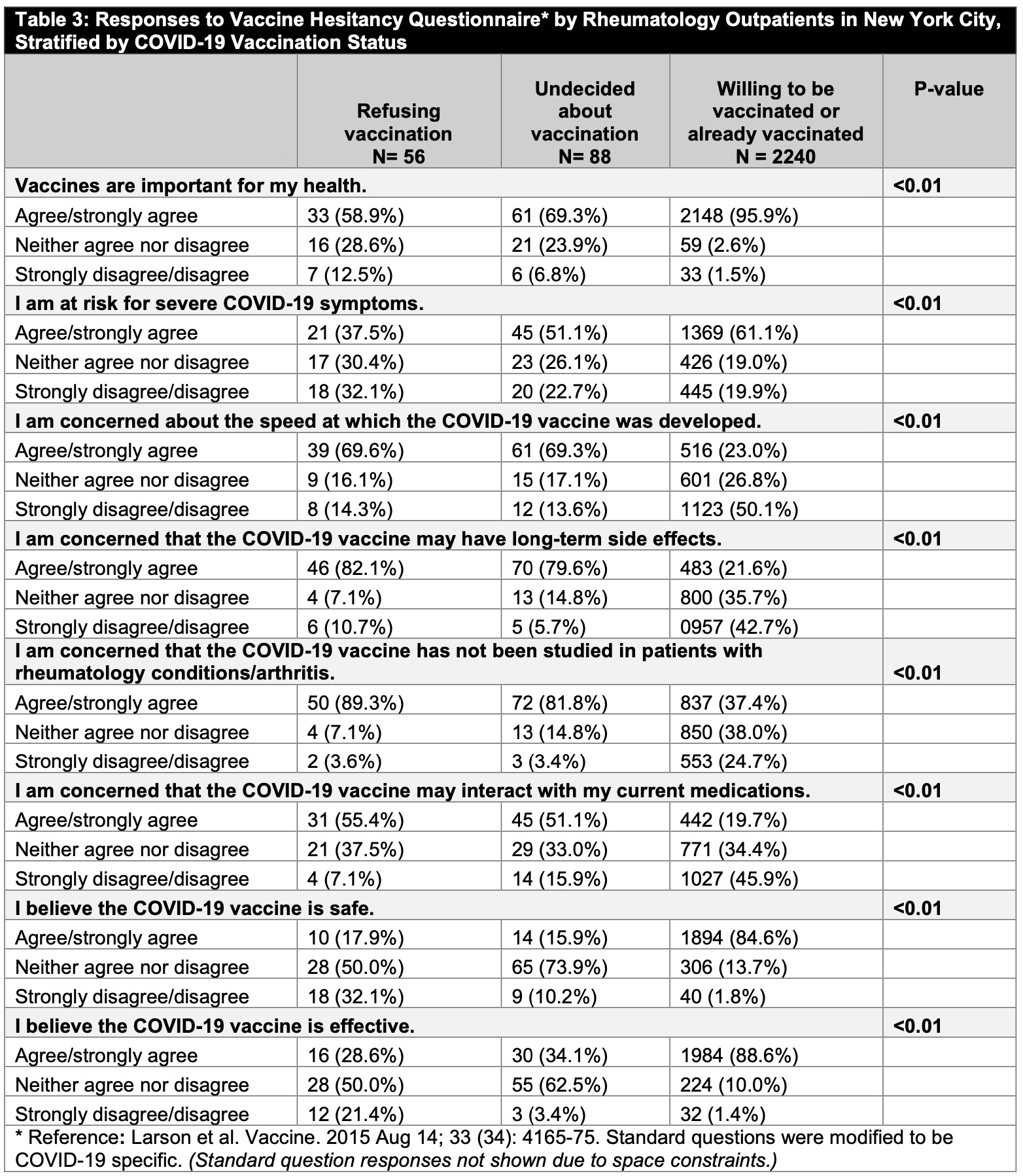
Results: Among 2,384 patients who completed the vaccine hesitancy questionnaire (31.8% response rate), 2,240 (94.0%) patients were willing/already received COVID-19 vaccination. 88 (3.7%) patients were ‘undecided’, and 56 (2.3%) reported vaccine refusal (Table 1). Compared to patients willing/already received vaccine, those refusing or undecided had lower mean ages (52.1y [SD 13.5] and 53.4 [SD 12.7] versus 61.4 [SD14.4]), higher percentage of Black, Hispanic/Latinx patients, patients with lower household income, and married/partnered patients; they had lower percentage with an advanced education degree (Table 1). Undecided patients were least likely to have received other immunizations during adulthood (Table 2), and those refusing the vaccine were most likely to have had a history of COVID-19 infection (33.9% versus 20.5% versus 9.1%, p< 0.01). SRD status differed between the groups, with SLE-like diseases being highest in those refusing the vaccine (p< 0.01). No differences in current use of immunosuppressive medications were observed. Vaccine questionnaire responses indicated that those refusing the vaccine were least likely to believe in the importance for health of vaccines in general, and in the safety or efficacy of the COVID-19 vaccine (Table 3). Patients refusing or undecided were most concerned about long-term vaccine side effects, lack of study in rheumatology patients, and the speed of vaccine development (Table 3).
Conclusion: Although vaccine hesitancy/refusal was only reported by 6% of respondents, our study provides useful insights into why rheumatology patients may refuse COVID-19 vaccination, including data that suggest the misperception that previous COVID-19 infection may mitigate the need for immunization.
To cite this abstract in AMA style:
Barbhaiya M, Schneider B, Levine J, Do H, Siegel C, Bykerk V, Feldman C, Jannat-Khah D, Mandl L. Factors Associated with COVID-19 Vaccine Hesitancy in Rheumatology Outpatients in New York City [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/factors-associated-with-covid-19-vaccine-hesitancy-in-rheumatology-outpatients-in-new-york-city/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/factors-associated-with-covid-19-vaccine-hesitancy-in-rheumatology-outpatients-in-new-york-city/