Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose:
Quantitative estimates of the duration and severity of cutaneous disease are lacking for adult dermatomyositis (DM) patients. The Cutaneous Dermatomyositis Disease Area and Severity Index (CDASI) is a validated instrument that quantifies cutaneous disease activity (CDASI-a), and allows for objective assessments of disease severity. Our aims were to estimate the percentage of DM patients with clinically significant skin inflammation who achieve clinical remission (CR) of skin disease during a 3-year follow-up period and to examine the relationship between skin disease course and selected clinical variables.
Methods:
Adult DM patients (age >18 years) seen at our outpatient clinic between May 15, 2007 and October 28, 2016 were considered for this study. DM was diagnosed using Bohan/Peter criteria, or, for clinically amyopathic patients, Sontheimer criteria. Patients were included if their initial CDASI-a score was greater than or equal to 12, and they had a minimum of 2 scores recorded 3 or more months apart. CR was defined as a CDASI-a less than or equal to 5 with no individual erythema score >1 and no ulcerations. Univariable and multivariable logistic regression analysis was performed using age, race, gender, amyopathic status, DM-associated malignancy, baseline CDASI-a, disease duration at baseline, time until first systemic therapy, autoantibody phenotype (Mi-2, TIF-1gamma, SAE1, MDA5, NXP2 or Ro52), and medication exposure as covariates. For selected variables, Kaplan-Meier plots were created and log-rank analysis used to compare curves.
Results:
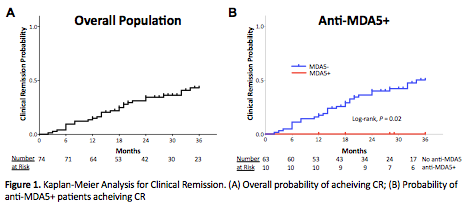
In total 74 patients met our inclusion criteria. The median duration of follow-up was 17.5 (11-28) months, with a median of 4 (3-6) months between CDASI scores. Overall, 36% of patients were treated with mycophenolate mofetil (MMF), 38% with antimalarials, 39% with methotrexate and 24% with IVIG. Twenty-eight patients (38%) entered CR within 3 years, and the overall probability of CR was 0.43 after 36 months (Figure 1A). The probability of CR was significantly higher for patients without anti-MDA5 antibodies (Figure 1B) as 0/10 anti-MDA5 patients entered CR. Increased age (OR 1.07, 95% CI 1.02-1.12; P=0.01), DM-associated malignancy (OR 14.46, 95% CI 2.18-96.07; P=0.006) and MMF (OR 6.00, 95% CI 1.66-21.78; P=0.0064) were significantly associated with CR in multivariable regression analysis.
Conclusion:
CR was relatively uncommon in our population, and even less common among anti-MDA5 patients, despite the use of aggressive systemic therapy. The positive association between MMF and CR suggests that MMF should be considered a first line agent for DM skin disease, while our overall results highlight the need for new therapies to more effectively treat skin disease in DM. Increased age and DM-associated malignancy were both associated with positive cutaneous outcomes, which has important prognostic significance.
To cite this abstract in AMA style:
Wolstencroft P, Chung L, Li S, Casciola-Rosen L, Fiorentino D. Factors Associated with Clinical Remission of Skin Disease in Dermatomyositis [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/factors-associated-with-clinical-remission-of-skin-disease-in-dermatomyositis/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/factors-associated-with-clinical-remission-of-skin-disease-in-dermatomyositis/