Session Information
Date: Friday, November 6, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster I: Clinical Manifestations
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Fatigue is commonly described in chronic illnesses, especially in auto-immune disorders such as systemic lupus erythematosus (SLE). We aim to study the prevalence of fatigue in SLE patients with NP symptoms attributed to major nervous system involvement in SLE and other attributions.
Methods: All patients visiting the tertiary referral center for NPSLE in the LUMC between 2007-2019 with the clinical diagnosis of SLE and age >18 years that signed informed consent were included in this study. Patients underwent a standardized multidisciplinary assessment, including two questionnaires: SF-36 (2007-2019) and multidimensional fatigue index (MFI, 2011-2019). Patients were classified as NPSLE in this study if NP symptoms were attributed to SLE and immunosuppressive or anticoagulant therapy was initiated, otherwise patients were classified as minor/non-NPSLE. The vitality (VT) domain of the SF-36 domain was used to assess fatigue, which generates a score from 0-100, 100 representing the complete absence of fatigue. Patients with a score more than one standard deviation (SD) removed from age-related controls of the Dutch general population were classified as fatigued; patients more than two SD removed were classified as extremely fatigued1. The MFI was also assessed, which consists of five subdomain scores between 0-20, leading to a total score between 0-100, 100 representing the most extreme fatigue. All scores are presented as mean and SD.
Results: 373 patients fulfilled the inclusion criteria and SF-36 questionnaires of 335 patients were available (90%). The majority of these patients was female (87%) and 97 were classified as NPSLE (29%). In NPSLE patients, average age was 41 years (SD: 13) and in minor/non-NPSLE the average age was 44 years (SD: 14). The average score of the SF-36 vitality domain was 35 (SD: 21) in NPSLE vs 34 (SD: 19) in minor/non-NPSLE. Overall, 75% of the patients were fatigued and 49% extremely fatigued in NPSLE vs 79% fatigued and 47% extremely fatigued in minor/non-NPSLE.
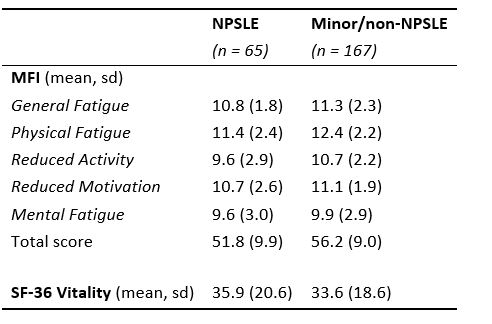
The MFI questionnaire was available for 230 patients, of which 65 patients were classified as NPSLE (28%). Table 1 depicts the scores of NPSLE and minor/non-NPSLE patients on the MFI subdomains.
Conclusion: Nearly half of all patients with SLE and NP symptoms are extremely fatigued compared to only 2.5% of the general Dutch population. Extreme fatigue is irrespective of NP attribution to SLE.
1. Aaronson et al. J Clin Epidemiol. 51, No. 11, pp. 1055–1068, 1998
 Fatigue in patients with NPSLE and minor/non-NPSLE
Fatigue in patients with NPSLE and minor/non-NPSLE
To cite this abstract in AMA style:
Monahan R, Fronczek R, Eikenboom J, Middelkoop H, Beaart-van de Voorde L, Terwindt G, van der Wee N, Huizinga T, Kloppenburg M, Steup-Beekman M. Extreme Fatigue in Patients with Systemic Lupus Erythematosus and Neuropsychiatric Symptoms [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/extreme-fatigue-in-patients-with-systemic-lupus-erythematosus-and-neuropsychiatric-symptoms/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/extreme-fatigue-in-patients-with-systemic-lupus-erythematosus-and-neuropsychiatric-symptoms/
