Session Information
Date: Sunday, November 8, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Comorbidities
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic lupus erythematosus (SLE) is a heterogeneous disease associated with increased morbidity and mortality, and severe SLE flares can lead to hospitalizations. Our objective was to apply machine learning methods to predict hospitalizations for SLE from electronic health record (EHR) data.
Methods: We identified 1,996 patients with SLE in a longitudinal academic medical center EHR-based cohort since 2016. Patients were identified with a previously validated SLE phenotype algorithm (PPV 92%) (Jorge A et al. Semin Arthritis Rheum 2019). K-means cluster analysis was used to identify groups of SLE patients with similar autoantibody patterns (dsDNA, SSA, SSB, Smith, RNP, and B2 glycoprotein 1 antibodies). The outcome of interest was hospitalization with a discharge diagnosis code of SLE (ICD10 M32, excluding M32.0, or ICD9 710.0) in the most recent year of follow up. We applied multiple machine learning methods to predict hospitalizations for SLE, including decision tree, random forest, logistic regression, and support vector machines. Candidate predictors were derived from coded EHR features and included demographics, laboratory tests, medications, ICD-9/10 codes for SLE manifestations (e.g., nephritis, acute lupus rash, and pericarditis), and healthcare utilization including specialist visits. We applied these methods to the overall SLE cohort and within clusters. The performance of each model was evaluated by sensitivity, specificity, accuracy, the F statistic, and the area under the receiver operator curve (AUC).
Results: Four distinct autoantibody clusters were identified (Table 1). SLE patients were 91% female, with mean age 52 years. Overall, 7.7% of patients were hospitalized for SLE in the last year of follow-up. Race/ethnicity and SLE manifestations varied among the clusters as did the proportion of patients with hospitalizations for SLE. Model performance was greatest within cluster 1, the largest cluster (Table 2). The most common predictors of SLE hospitalizations overall from the various machine learning methods included age, hemoglobin/hematocrit, ESR, and albumin. Top 5 predictors for SLE hospitalizations varied among clusters of SLE patients (Table 3).
Conclusion: We have demonstrated that machine learning methods can be used to predict SLE hospitalizations and to identify predictors of these events. Future work will incorporate natural language processing of narrative text to capture additional predictors of SLE hospitalizations.
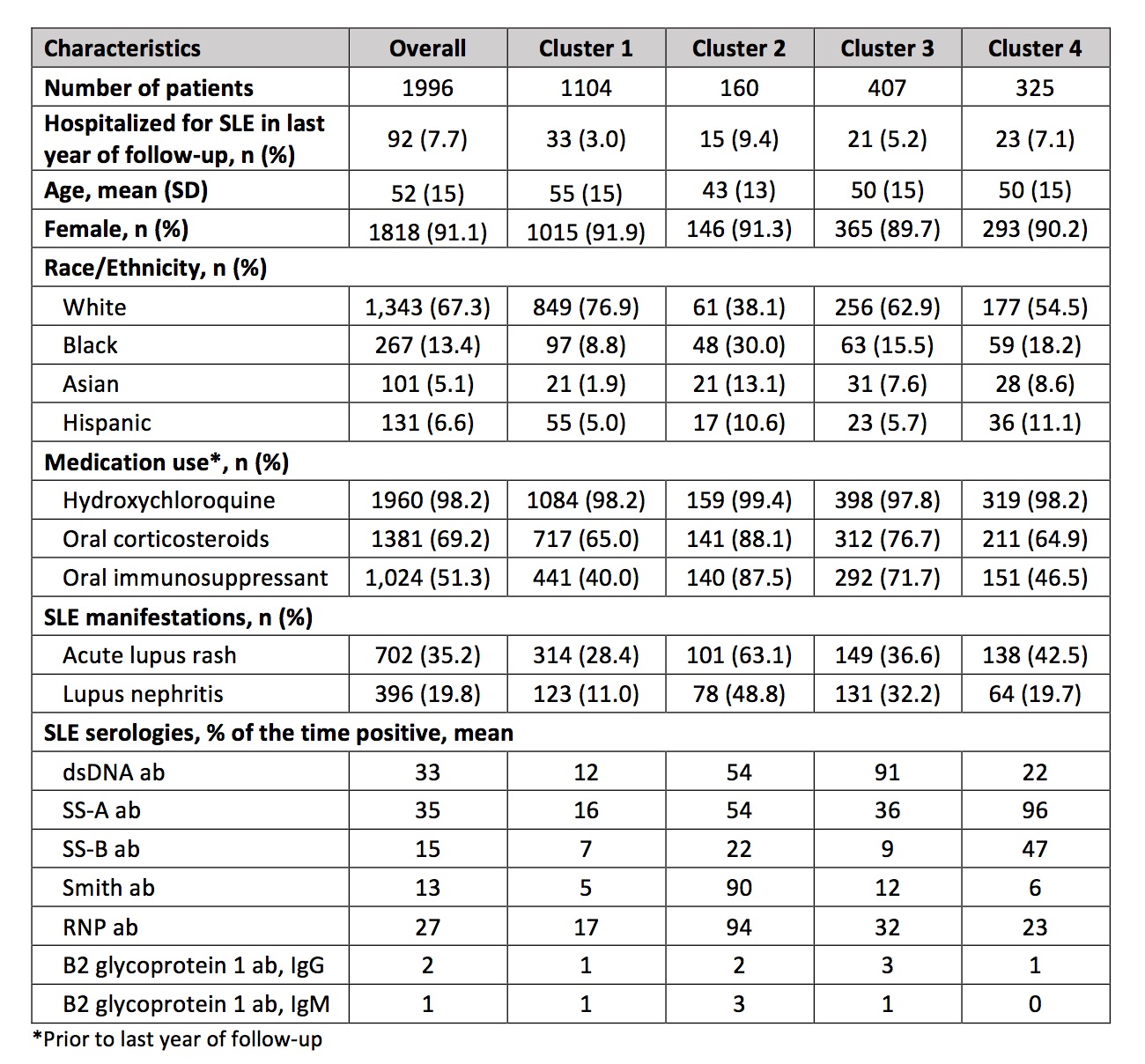 Table 1. Characteristics of Systemic Lupus Erythematosus Patients Overall and by Serologic Clusters
Table 1. Characteristics of Systemic Lupus Erythematosus Patients Overall and by Serologic Clusters
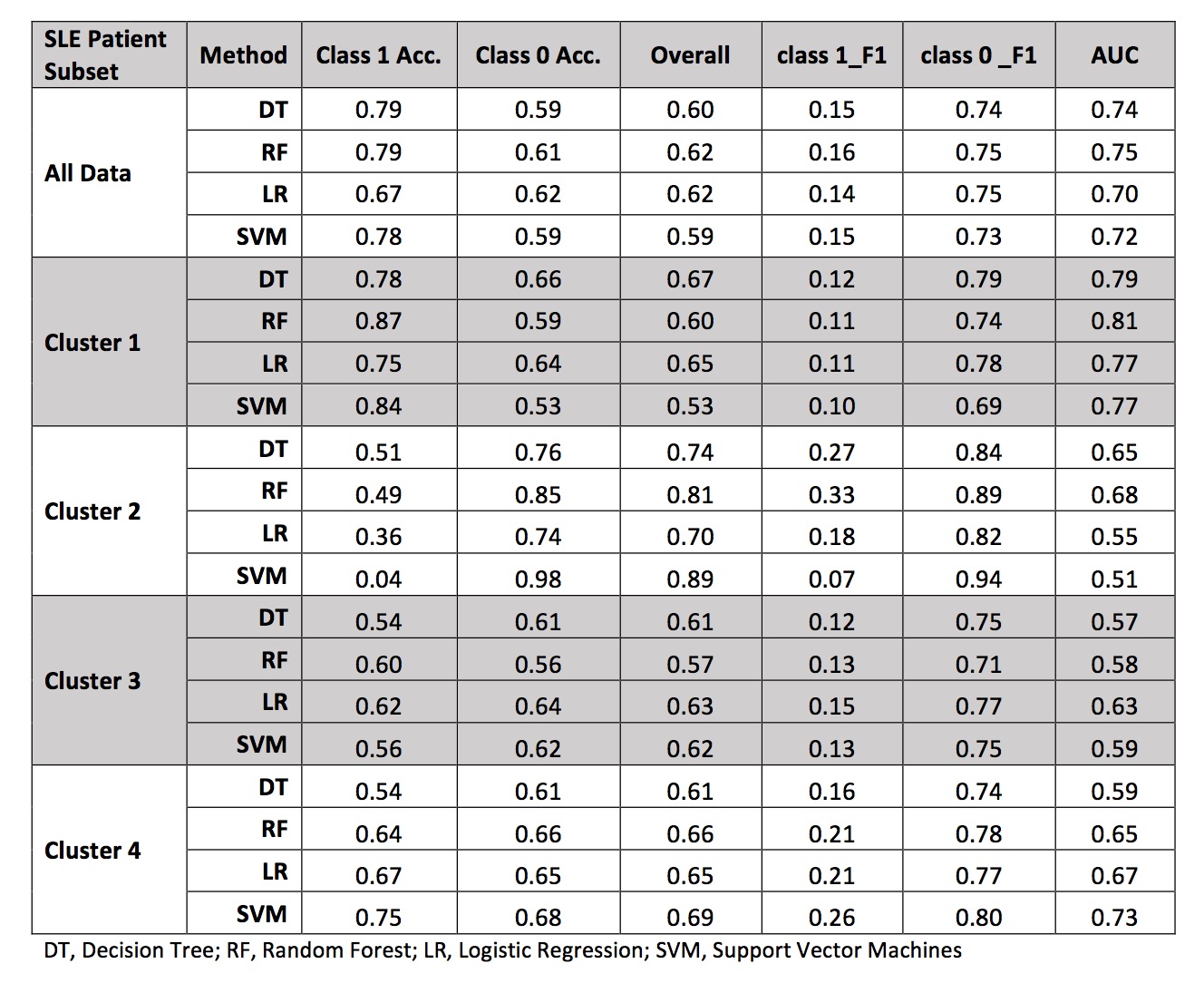 Table 2. Performance Characteristics of Four Machine Learning Models in Predicting Hospitalization for Systemic Lupus Erythematosus, Overall and by Cluster
Table 2. Performance Characteristics of Four Machine Learning Models in Predicting Hospitalization for Systemic Lupus Erythematosus, Overall and by Cluster
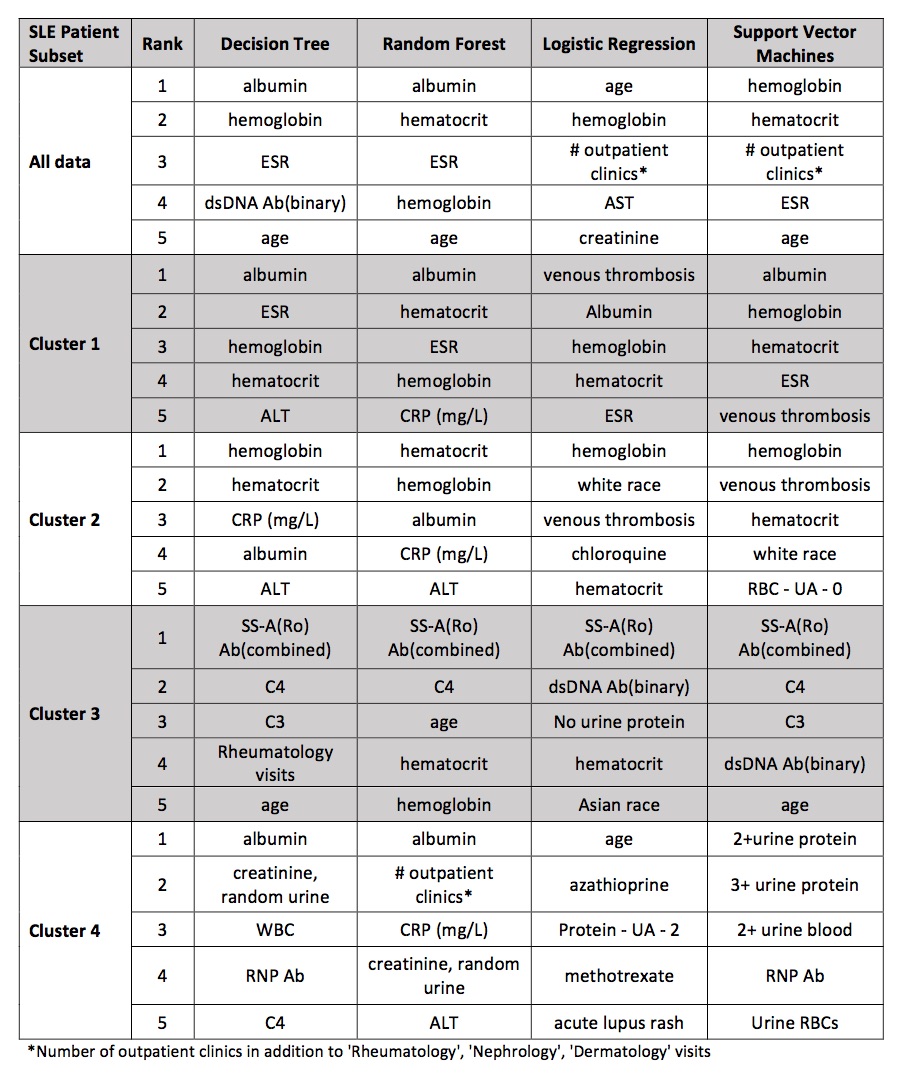 Table 3. Comparison of Top Five Predictive Features of Four Machine Learning Models
Table 3. Comparison of Top Five Predictive Features of Four Machine Learning Models
To cite this abstract in AMA style:
Jorge A, Wu Z, Chowdhury T, Zhao Y. Exploration of Machine Learning Methods in Predicting Systemic Lupus Erythematosus Hospitalizations [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/exploration-of-machine-learning-methods-in-predicting-systemic-lupus-erythematosus-hospitalizations/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/exploration-of-machine-learning-methods-in-predicting-systemic-lupus-erythematosus-hospitalizations/
