Session Information
Date: Tuesday, November 14, 2023
Title: (2257–2325) SLE – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with systemic lupus erythematosus (SLE) have a 1.85-fold higher risk of all-cause mortality and a 2.74 fold higher risk of infection-related mortality compared with controls. In addition, infection is responsible for up to 45% of hospitalization and 65.8% of death. However, few studies had developed a prediction tool for hospitalized infection in patients with SLE using electronic medical records (EMR). Therefore, we aimed to develop predictive models for hospitalized infection in patients with SLE in a medical center in central Taiwan.
Methods: Using EMR data of patients with SLE from the Taichung Veterans General Hospital during the period of 2012–2022, we conducted five machine learning (ML) models, including extreme boosting (XGBoost), random forest (RF), logistic regression (LR), support vector machine (SVM) and K nearest neighbor (KNN). The ratio between training/testing was 80/20. We used the SHAP summary plot to illustrate the strength and the direction of associations between key features and 30-day risk of hospitalized infection. We performed the receiver operating characteristic (ROC) analysis, calibration curve and decision curve analysis to determine discrimination, accuracy and applicability of the predictive ML modes in the testing datasets.
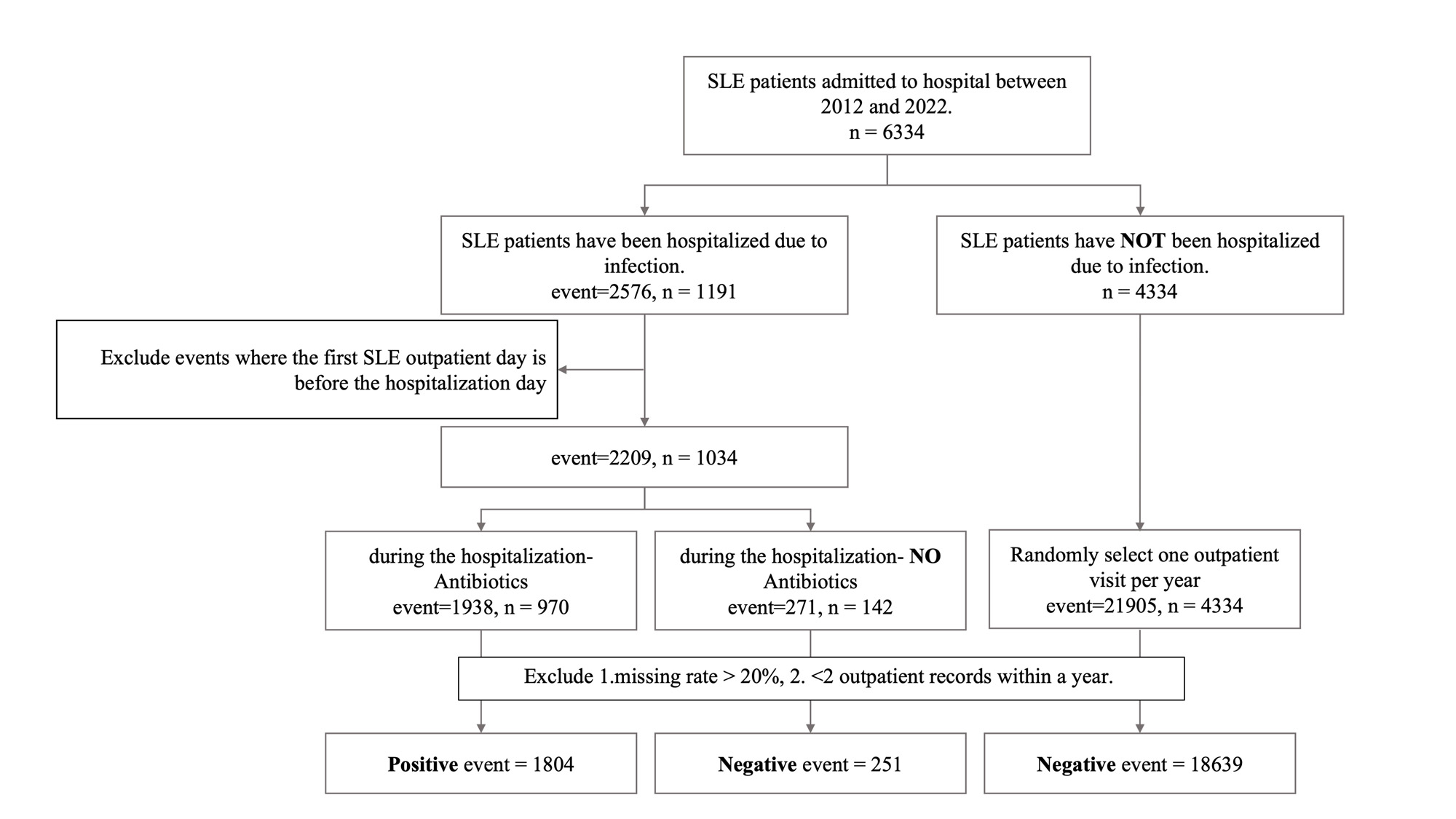
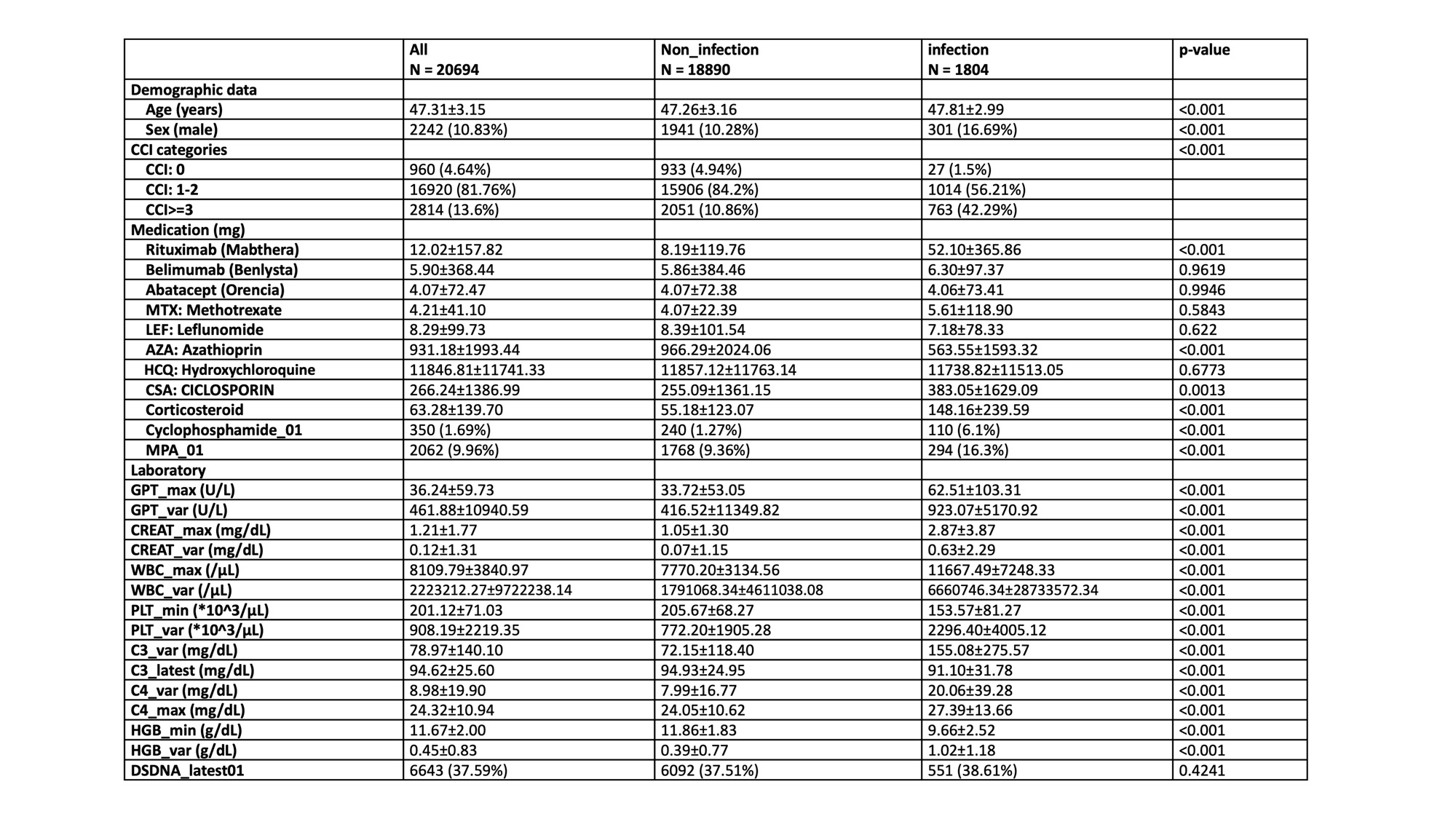
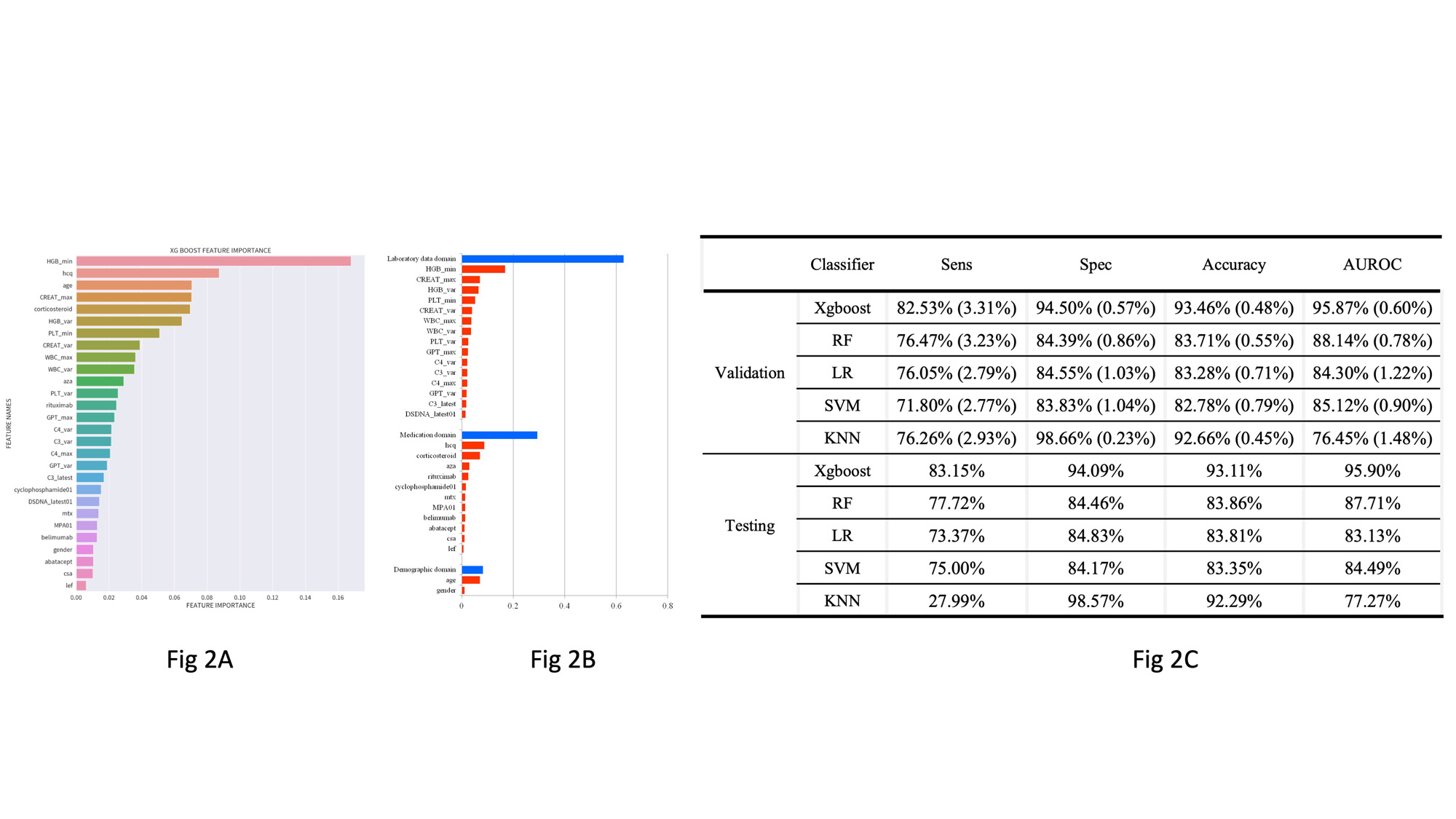
Results: Figure 1 showed the flowchart of subject enrollment. A total of 5368 patients with SLE with at least two ambulatory visits were included. Table 1 summarizes characteristics of patients with and without hospitalized infection. We finally included 28 features of four domains (demographics, laboratory data within one year before the index date, comorbidities in prior one year, and cumulative dose of medications in prior 3 months [9 months for rituximab]) based on feature importance in the ML models (Fig 2A). Fig 2B showed cumulative relative feature importance of top 28 features categorized by main clinical domains in predicting 30-day hospitalized infection. As shown in Fig 2C, XGBoost showed the best performance among the five ML models with a sensitivity of 83.15%, a specificity of 94.09%, an accuracy of 93.11% and an area under curve (AUC) in ROC analysis of 95.9% in the testing datasets. Because laboratory data domain provides the largest portion of feature importance, after exclusion of 11 medication domain features, we re-conducted ML models using 15 laboratory data domain features and 2 demographic domain features and found the XGBoost model still revealed the best performance with an accuracy of 91.91% and an AUC in ROC of 93.94% (data not shown).
Conclusion: We developed explainable ML models to predict hospitalized prediction in patients with SLE using 10-year EMR data from a medical center in Taiwan.
To cite this abstract in AMA style:
Chen H, Huang W. Explainable Machine Learning to Predict Hospitalized Infection in Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/explainable-machine-learning-to-predict-hospitalized-infection-in-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/explainable-machine-learning-to-predict-hospitalized-infection-in-patients-with-systemic-lupus-erythematosus/