Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose:
Rheumatoid arthritis (RA) is a known risk factor for the development of cardiovascular disease (CVD). However, the influence of RA on the prognosis after initial diagnosis and treatment for coronary artery disease (CAD) is unknown.
Objective:
To examine the risk of major cardiovascular events (MACE) and all-cause mortality among RA and non-RA patients after referral to cardiac computed tomography (CCT) due to symptoms suggestive of CAD.
Methods:
This was a follow-up study, using data from the Western Denmark Heart Registry [1] covering all diagnostic procedures in a catchment area with approximately 3.3 mill. inhabitants. The register provides information on clinical variables such as smoking, severity of stenosis and calcium score. Information on RA diagnosis and co-variates were identified through individual-level linkage of nationwide administrative registers.
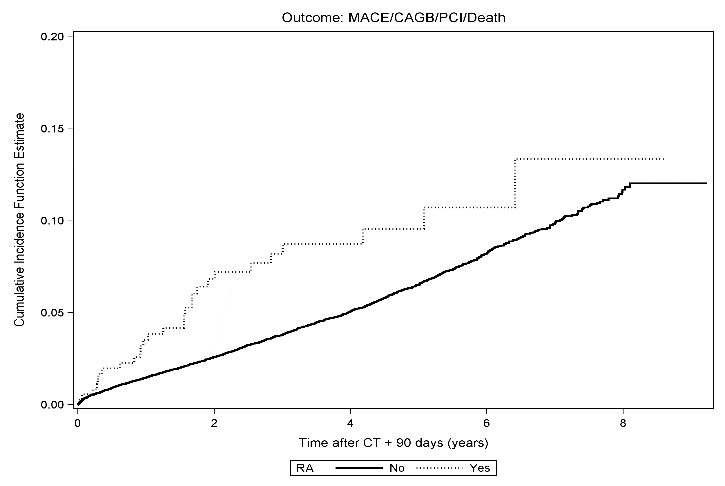
Outcome measures were MACE alone and a combined outcome (CO) including MACE, coronary artery bypass grafting, percutaneus coronary intervention, and all-cause mortality. Median time until events or censoring were 3.5 years (min/max: 0.0: 9.2).
In the studied region, RA-flares are controlled through escalation of disease modifying drugs and intra-articular or intramuscular glucocorticoid injections (GCI). Hence, the number of times a patient had received GCIs 3 years prior to the CCT were used as a surrogate marker of disease activity. Analyses were performed for overall RA and the serological subtypes: ‘seropositive RA’(ICD-10: M05) and ‘other RA’(ICD-10: M06).
Cox proportional hazard models were used to examine the association between RA and non-RA patients and the outcomes.
Results:
We included 42,257 patients, and identified 358 (0.8%) patients with RA. The incidence rate for revascularization, not related to the initial diagnosis, in RA and non-RA patients was 3.4 (95% CI 1.3-9.0) vs. 3.7 (95%CI 3.7-4.1)/1000 person-years. For both the CO and MACE an increased risk was seen in RA compared to non-RA (CO: hazard ratio (HR): 1.35 (95% CI: 0.93-1.96), MACE: HR 1.94 (95% CI: 1.18-3.19)). The risk was higher among patients who had received GCI more than one time during 3 years prior to the CT (CO: HR: 1.80 (95% CI: 1.1-3.0), MACE: HR 3.02 (95% CI: 1.62-5.65)) and in patients with sero-positive RA (CO: HR: 1.42 (95% CI: 0.93-2.16), MACE: HR: 2.45 (95% CI: 1.47-4.08)) (Fig. 1).
Conclusion:
We found a strong association between RA and cardiovascular events in the period after the initial diagnosis and treatment in this cohort of patients with a-priori risk of CAD referred for cardiac CT . These findings support that RA per se, but in particular, sero-positivity and inflammation related to flares increase the risk of CVD and mortality.
1. Nielsen LH, Bottcher M, et al. The Western Denmark Cardiac Computed Tomography Registry: a review and validation study. Clinical epidemiology 2014.
To cite this abstract in AMA style:
de Thurah A, Trolle Andersen I, Bugge Tingaard A, Therkildsen J, Hammerich Riis A, Böttcher M, Hauge EM. Excessive Risk of Major Cardiovascular Events in Sero-Positive Rheumatoid Arthritis and in Patients with Active Disease [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/excessive-risk-of-major-cardiovascular-events-in-sero-positive-rheumatoid-arthritis-and-in-patients-with-active-disease/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/excessive-risk-of-major-cardiovascular-events-in-sero-positive-rheumatoid-arthritis-and-in-patients-with-active-disease/