Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic lupus erythematosus (SLE) is a heterogeneous disease that disproportionately affects women, racially and ethnically minoritized populations, and people of lower socioeconomic status (SES). Though SLE diagnosis and treatment have improved, United States health disparities persist. Our prior urban center study showed that living in disadvantaged neighborhoods was one of the strongest factors associated with fewer SLE visits and labs. The current study aimed to expand upon findings by examining SLE across rural, urban and suburban academic institutions in the state to identify care gaps and damage.
Methods: Our cohort included patients with prevalent SLE and at least one rheumatology and one primary care visit at one of three tertiary care centers in a Midwest state: urban, suburban, and rural populations. Process measures included receipt of any hydroxychloroquine (HCQ) (or documented contraindication or intolerance) and HCQ adherence defined as prescriptions covering >/=80% of calendar days (2014). Primary outcomes were time to new SLICC damage index (SDI) events or death 1/1/2015-12/31/2020. Processes and outcomes were reported by race, ethnicity, and Area Deprivation Index (ADI), a composite of 17 variables depicting neighborhood disadvantage. Data were analyzed using descriptive statistics and Cox proportional-hazards models.
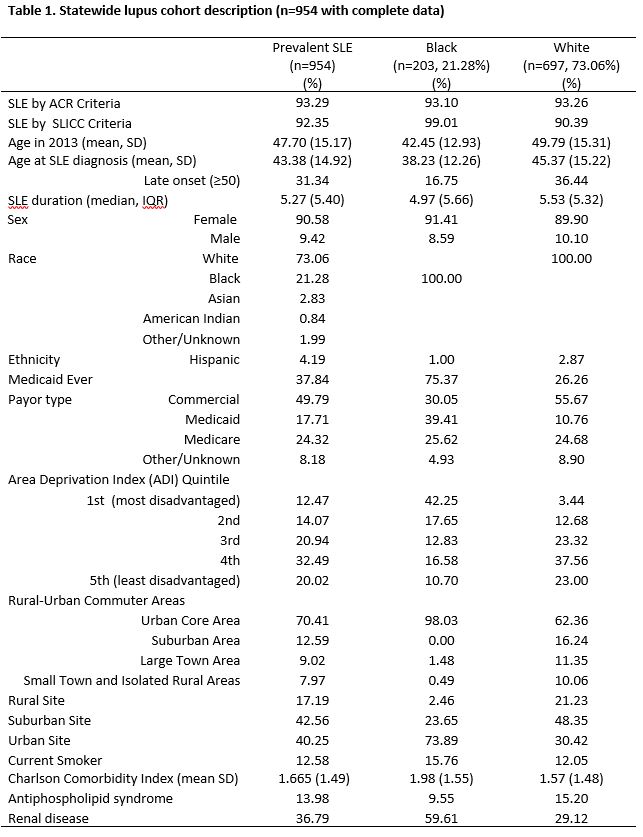
Results: A total of 954 SLE patients were identified. Most were female (90.58%) and White (73.06% vs 21.28% Black; Table 1). Average age at SLE diagnosis was 43.38 (SD 14.92). Patients of Black race were diagnosed at an earlier age (38.23, SD 12.26 vs 45.37, 15.22 White). Most patients of Black race were from the urban site (73.89%). Black patients also had a much higher representation in the most disadvantaged ADI neighborhood quintile (42.25% vs 3.44% White). Antiphospholipid syndrome was more prevalent in White patients (15.20% vs. 9.5% Black); renal disease more prevalent in Black patients (59.61% vs. 29.12% White).
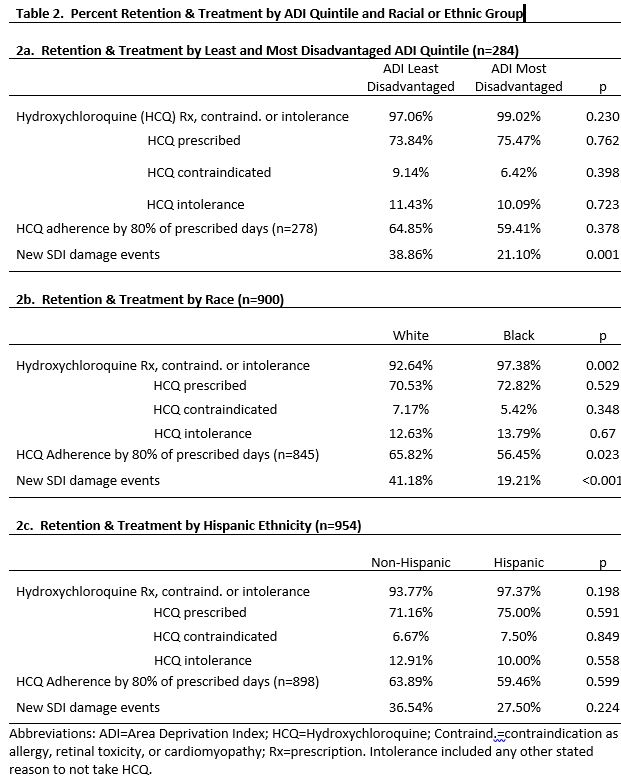
No statistically significant differences in HCQ use were noted by ADI or ethnicity, but compared to White patients, those of Black race had higher rates of prescription or contraindication for HCQ (97.38% vs 92.64 White%, p=0.002). Black patients had 9.37% lower adherence defined by prescriptions covering >/=80% of days (56.45% v. 65.82%, p=0.023). Yet, HCQ adherence did not predict SDI damage (38% with vs 33% without >/=80% HCQ days). Table 2 shows more damage in White and less disadvantaged. Limits include possible selection or follow up bias, and adherence by prescribing data.
Conclusion: SLE patients of Black race were much more likely to live in the most disadvantaged ADI quintile in this cohort. Black patients were more likely prescribed HCQ but less likely to have >/= 80% of days prescribed than White patients. In sum, data showed no significant disparities in HCQ use by neighborhood ADI or ethnicity at these tertiary centers, but did show lower prescribed days covered for Black patients possibly reflecting adherence or prescribing differences. No changes in subsequent damage correlated with HCQ prescribed coverage. Future larger studies should investigate long-term associations between damage and adherence and prescribing.
To cite this abstract in AMA style:
Cormier J, Sutherland B, Jiang Y, Gazeley D, Katz J, Parikh S, Torres C, Charles E, Yu A, Elwert F, Bartels C. Examining Hydroxychloroquine Prescribing and SLE Damage in a Statewide Lupus Cohort [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/examining-hydroxychloroquine-prescribing-and-sle-damage-in-a-statewide-lupus-cohort/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/examining-hydroxychloroquine-prescribing-and-sle-damage-in-a-statewide-lupus-cohort/