Session Information
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: The last decade has seen dramatic shifts in pharmacotherapy for rheumatoid arthritis (RA) with the increasing availability of biologic and targeted synthetic DMARDs (b/tsDMARDs). While newer drugs have improved patient outcomes, disparities in access and use persist. This study aims to analyze the changes in b/tsDMARD use from 2014 to 2023 in a national registry and examine the patient factors associated with the adoption of these newer drugs.
Methods: Data derive from RISE, a national, EHR-enabled rheumatology registry. Included patients were ≥ 18 years old and had 2 ICD codes for RA 30 days apart between 2014 and 2023. Patients’ b/tsDMARD use and disease activity scores were extracted after the index date, defined as the date of the second RA code. Patient characteristics included age, sex, race and ethnicity, area deprivation index, and insurance. To examine trends in b/ts DMARD use, we performed a run chart analysis in which the outcome was the percentage of patients using each category of b/tsDMARD among all RA patients with a visit in a given month after their index date. Using multi-level logistic regression, in which we accounted for repeated measures within patients, and in which patients were clustered within practices, we assessed the association between the use of any b/tsDMARD (yes/no) and patient characteristics. Additional analyses were conducted adjusting for RA disease activity scores (available for 55% of observations). Finally, we analyzed whether there were interactions between year and several variables (age, race and ethnicity, and ADI) to understand if the relationships between these variables changed over time.
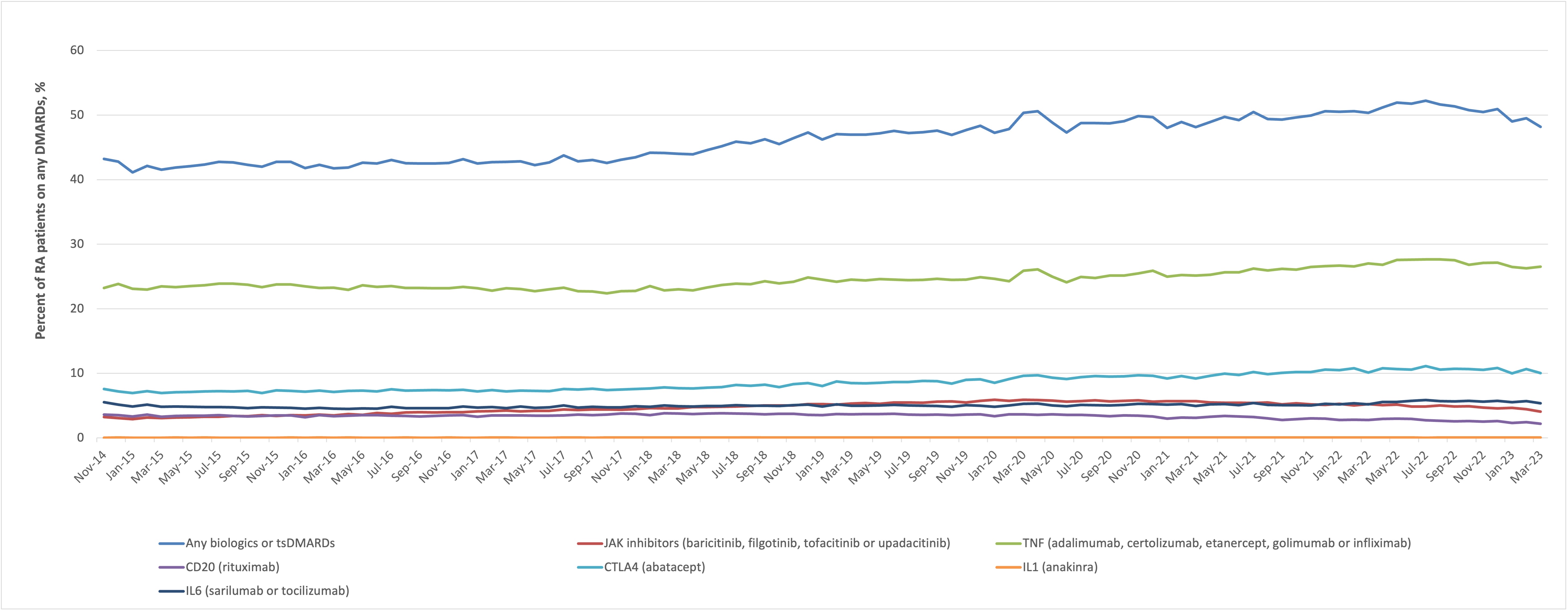
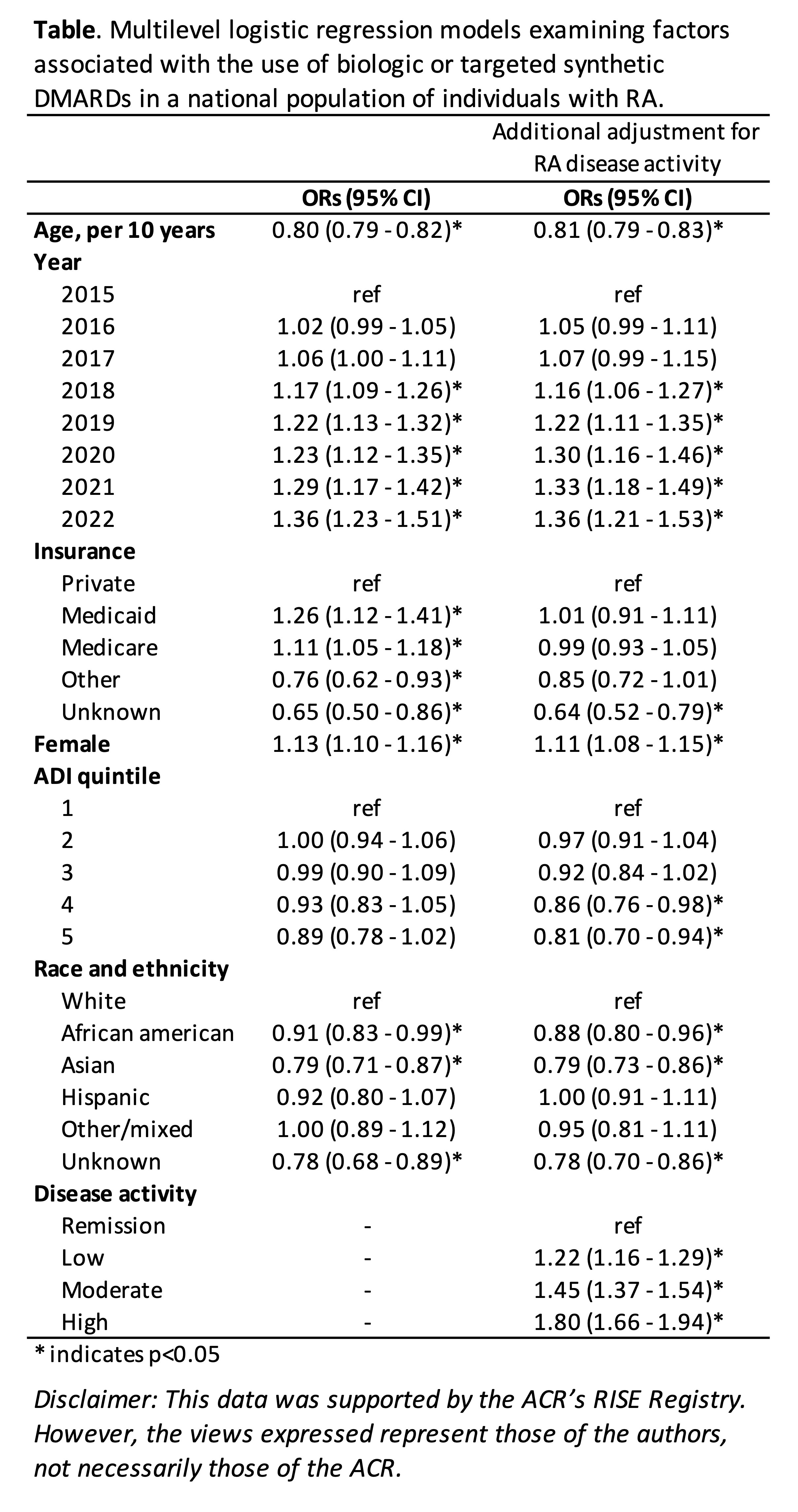
Results: A total of 360,162 individuals with RA were included, with a mean (SD) age of 60 (14) years. 77% were female, 66% non-Hispanic white, and most had either Medicare (45%) or private (36%) insurance. We observed slowly increasing use of b/tsDMARDs over the decade of observation (Figure); 37% of individuals used b/tsDMARDs in 2014 rising to almost 50% in 2023. The most commonly used drug categories were TNFi and abatacept throughout the study period. (Figure). Anti-CD20 use rose until 2020 when a mild decrease occurred, corresponding to the COVID-19 pandemic. In adjusted analyses, those who were older, Asian or Black (vs. white), or living in areas with more socioeconomic deprivation were less likely to use b/tsDMARDs. Similar results were observed after adjusting for disease activity (Table). There were no significant interactions between age, ADI, or race and ethnicity, and year.
Conclusion: The last decade has seen significant shifts in treatment among U.S. patients with RA, with growing use of b/tsDMARDs. However, use of newer therapies was lower among older individuals, those living in areas of greater socioeconomic deprivation, as well as among Asian and Black individuals, differences that have neither widened nor narrowed over time. Whether these differences represent disparities in access to therapies warrants further investigation.
To cite this abstract in AMA style:
Li J, Schmajuk G, Yazdany J. Evolution of Rheumatoid Arthritis Pharmacotherapy: A Ten-Year Analysis of Biologic and Targeted Synthetic DMARD Use and Its Predictors in a National Sample of Rheumatology Practices [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/evolution-of-rheumatoid-arthritis-pharmacotherapy-a-ten-year-analysis-of-biologic-and-targeted-synthetic-dmard-use-and-its-predictors-in-a-national-sample-of-rheumatology-practices/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/evolution-of-rheumatoid-arthritis-pharmacotherapy-a-ten-year-analysis-of-biologic-and-targeted-synthetic-dmard-use-and-its-predictors-in-a-national-sample-of-rheumatology-practices/