Session Information
Date: Monday, November 8, 2021
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Spinal involvement in Rheumatoid arthritis (RA) is limited to the upper region of the cervical spine which leads to cervical spine instability (CSI); anterior atlantoaxial subluxation (aAAS), vertical subluxation (VS), and subaxial subluxation (SAS). In this study, we aimed to evaluate the frequency of cervical involvement and the associated risk factors in patients with RA.
Methods: Two hundred-forty RA patients were recruited consecutively in this single center cross-sectional study. All participants met the ACR 2010 classification criteria. Demographics, laboratory data, patient and physician reported outcomes were collected using by a structured form. Tender and swollen joint count was assessed by the same rheumatologist. Radiographs of the cervical spine were obtained in flexion, extension, neutral position of the neck at the same visit. The presence of erosions on the hand and foot radiographs in the last year was also assessed. A diagnosis of aAAS was based on the distance between the anterior aspect of the dens and, the posterior aspect of the anterior arch of the atlas was > 3 mm during flexion (Figure 1). Vertical subluxation was recorded as present if the tip of the odontoid peg lay more than 4.5 mm above the line described by McGregor. SAS is diagnosed if a vertebra has moved 3 mm or more in relation to the next vertebra when measured from the posterior line of the vertebral bodies. All cervical spine radiographs were evaluated separately by two readers blinded to all clinical data of patients at the end of the study. There was very good agreement between the two readers [interobserver reliability: intraclass correlation coefficent (ICC) for GA: 0.88 (95% CI: 0.43 – 0.97), ICC for HC:0.80 (95% CI: 0.14 – 0.95); intraobserver reliability: ICC:0.89 (95 % CI: 0.47-0.97)].
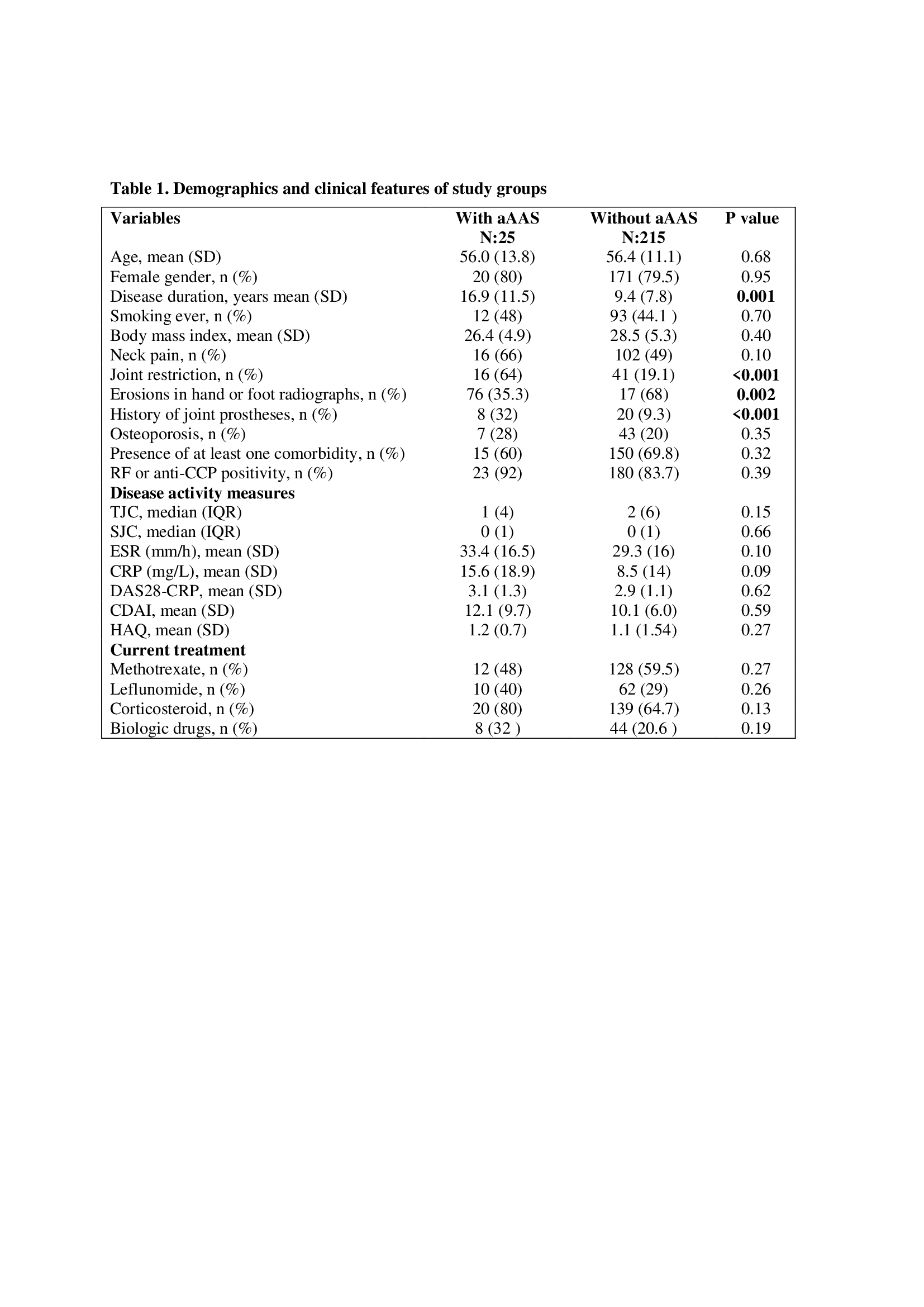
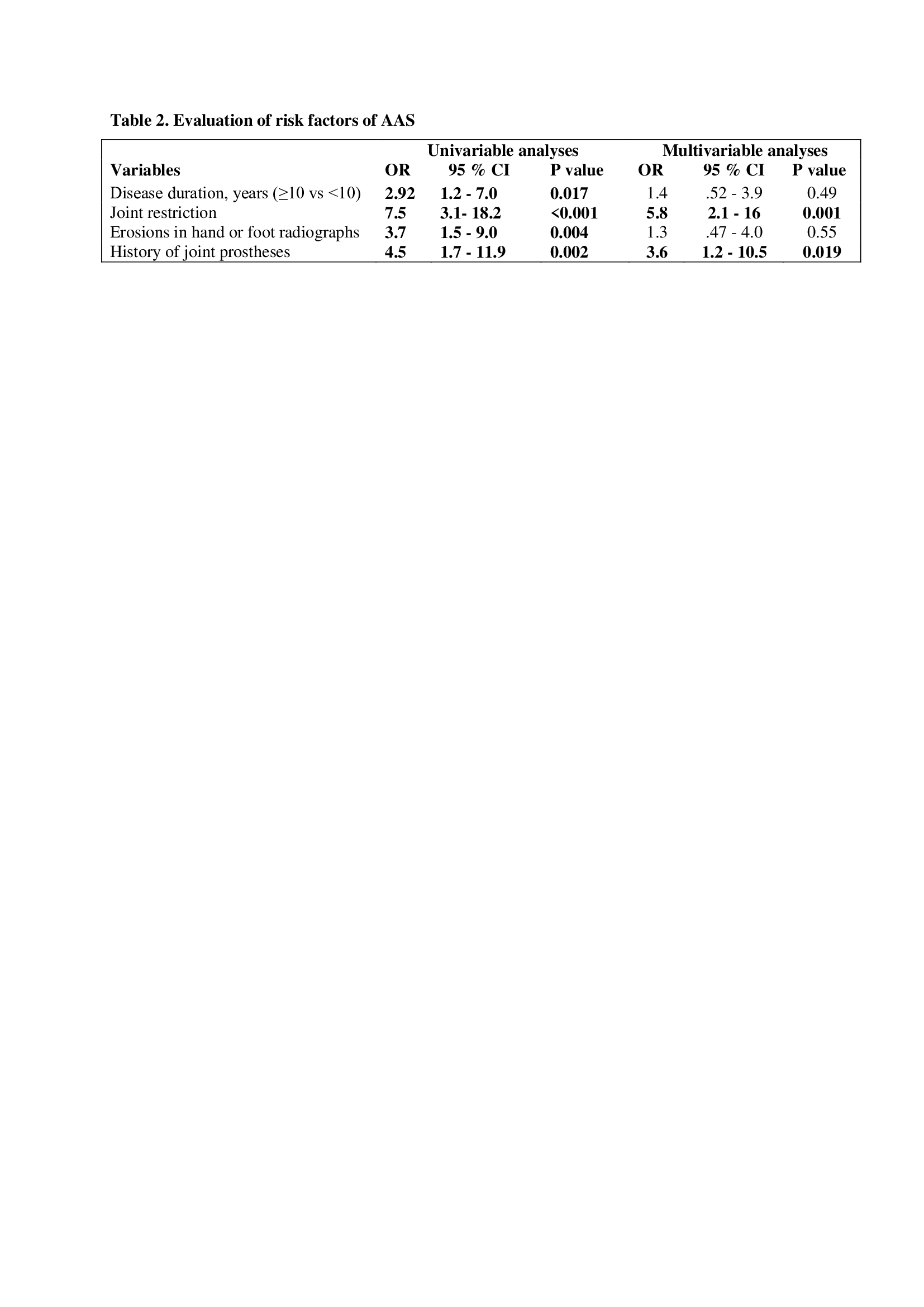
Results: One hundred ninety-one (79.6 %) of the 240 patients were female, and the mean age was 56.4 ± 11.4 years with a mean of 10.2 ± 8.5 years of mean disease duration. Two hundred and three (84.6 %) of the participants were seropositive (RF or anti CCP) and erosion was detected in 93 patients’ hand or foot radiographs. aAAS was reported in 25 (10.4 %) patients. Only one patient had combination of aAAS and VS. We could not detect any SAS. Age and gender were found similar in patient with or without aAAS and the other demographics and clinical characteristics were summarized in table 1. One in three patients with aAAS had no neck pain. Biologic drugs treatment and presence of osteoporosis was more common in the aAAS group but not reach a statistical difference (32% vs 20%, p:0.19; 28% vs 20%, p:0.37, respectively). Patient with aAAS had longer disease duration, more frequently erosion, joint restriction and history of joint prostheses (Tablo1 and 2). In the multivariate regression model, joint restriction [OR: 5.8 (95% CI: 2.1-16.0)], and history of joint prostheses [OR:3.6 (95% CI: 1.2-10.5)] was found independently predictors of the presence of aAAS.
Conclusion: aAAS was found the most common cervical involvement type in RA in this study. Longer disease duration, presence of erosion, joint restriction and prostheses was associated with aAAS. Even if there is no neck pain, cervical involvement should be kept in mind especially in the established disease.
To cite this abstract in AMA style:
Alp G, Cinaklı H, Solmaz D, OTMAN E, Ediboglu E, Erpek E, Akar S. Evaluation of the Cervical Involvement Frequency and Associated Risk Factors in Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/evaluation-of-the-cervical-involvement-frequency-and-associated-risk-factors-in-patients-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/evaluation-of-the-cervical-involvement-frequency-and-associated-risk-factors-in-patients-with-rheumatoid-arthritis/