Session Information
Date: Monday, November 13, 2023
Title: (1442–1487) SLE – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic lupus erythematosus (SLE) is an autoimmune disease associated with a high degree of variability at onset, which may make SLE diagnosis challenging, with an estimated time between onset of symptoms and diagnosis of 24 months[1]. Moreover, in SLE early diagnosis and therapeutic advances have led to better improve outcomes, and achievement of persistent low disease activity and/or remission have been associated with reduced long-term organ damage. The aim of this study was to evaluate the changes in the onset pattern of SLE in demographic and clinical terms, and for changes in assessment and therapy at diagnosis and during the f-up.
Methods: Medical records of 125 patients diagnosed between 1970 to 2019 and regularly followed up were reviewed. Patients were divided into 4 groups based on the year of diagnosis: 1970-’89, 1990-’99, 2000-’09, 2010-’19. Disease activity, cumulative organ damage and remission were recorded according to validated indices (SLEDAI-2K, SLEDAS, SLICC Damage Index, LLDAS and DORIS) at the time of diagnosis (T0) and at 1 (T1), 5 (T2) and 10 (T3) years after. GCs (both in absolute terms and daily dosage), hydroxychloroquine (HCQ) and DMARDS use were also evaluated at the same time points. Qualitative variables were compared with Chi-Squared or Fisher’s exact test, quantitative variables with one-way Anova or Mann-Whitney test
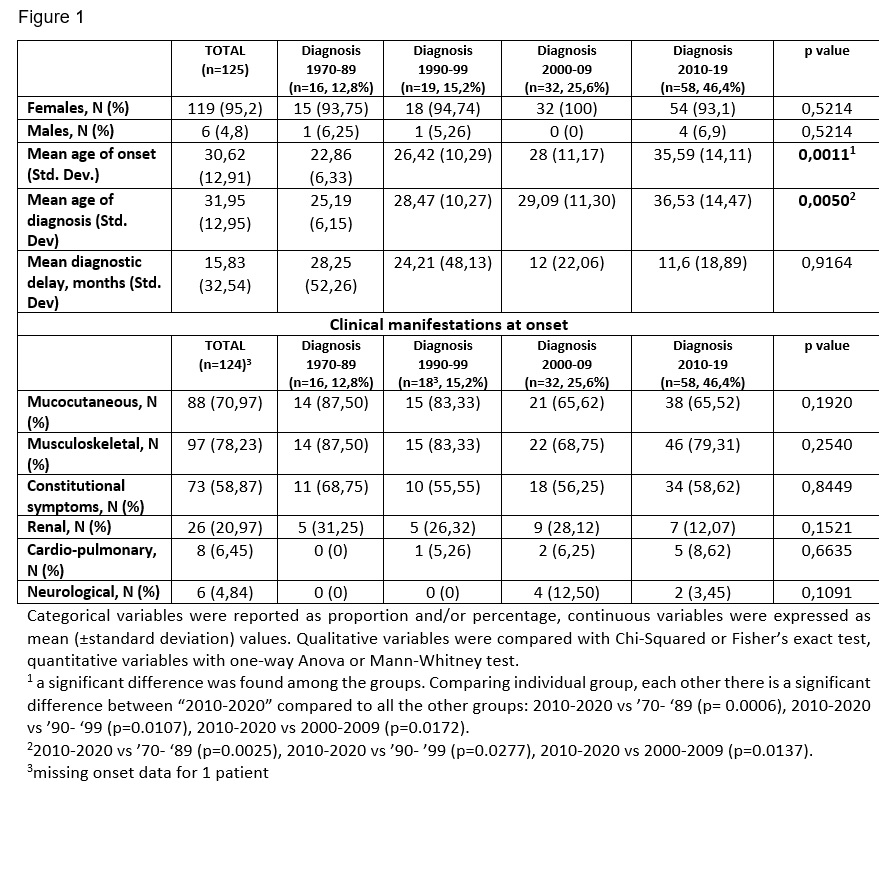
Results: Our cohort consisted of 119 females and 6 males; the mean age of onset was 30,62 years and the mean age of diagnosis was 31,95. Mean age of onset, and consequently mean age of diagnosis, has significantly increased in different groups (p=0,0011) (Figure 1). We observed a decreasing trend in the mean diagnostic delay from 28,25 months to 11,6 although without statistical significance (p=0,5015). Concerning the clinical presentation at onset, the most frequent symptoms observed were musculoskeletal (78,23%) and mucocutaneous (70,97%).
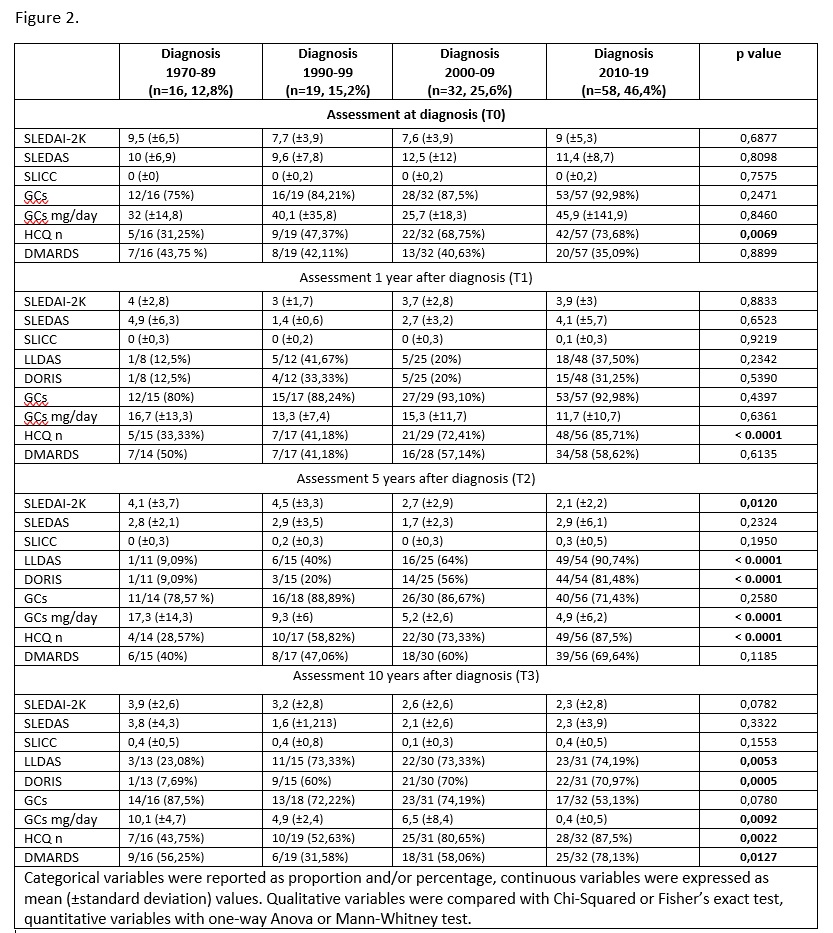
Evaluating patients at the time of diagnosis through the different decades (Figure 2), no significant changes were found in disease activity or damage, nor in the treatment except in the early use of HCQ: from less than 50% before 1999, to more than 70% of patients (p=0.0069). As for disease activity, a significant variation in the different decades appears at T2, with a reduction in SLEDAI (p=0.0120) and a higher number of patients reaching LLDAS and DORIS (both p< 0.0001); similar results were confirmed at T3 for both indexes. As for the use of GCs, no difference was observed in number of patients treated, although a significant reduction in GCs daily dose was observed at T2 and T3 (p< 0.0001 and p=0.0092 respectively). Finally, in patients with a more recent diagnosis, an increased use of HCQ (p< 0.0001 for T2 and p=0.0022 for T3) and DMARDS (p=0.0127 at T3) was observed during f-up
Conclusion: Our preliminary data demonstrated a progressive increase in the mean age at the onset of SLE over the years. However, this increase does not deviate from the mean age range defined in the literature [2].Moreover, our data reflect the therapeutic improvements of the past decades characterized by use of lower doses of GCs, increased use of HCQ and DMARDS and faster achievement of LLDAS and DORIS.
[1] Kapsala et al, CER 2023
[2] Sassi Rh et al, Clin Rheumatol 2017
To cite this abstract in AMA style:
Fredi M, Della Pina S, Barison C, Orlandi C, Tedeschi M, Chiara M, Nalli C, Franceschini F. Evaluation of Changes in SLE Patients’ Phenotype at Disease Onset, and Assessment of Disease Activity, Damage and Therapy at Diagnosis and During Follow up in the Last Forty Years: Preliminary Data of a Single Center Experience [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/evaluation-of-changes-in-sle-patients-phenotype-at-disease-onset-and-assessment-of-disease-activity-damage-and-therapy-at-diagnosis-and-during-follow-up-in-the-last-forty-years-preliminary/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/evaluation-of-changes-in-sle-patients-phenotype-at-disease-onset-and-assessment-of-disease-activity-damage-and-therapy-at-diagnosis-and-during-follow-up-in-the-last-forty-years-preliminary/