Session Information
Date: Monday, November 13, 2023
Title: (1155–1182) Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: ILD is a major cause of morbidity and mortality in IIM. The diagnosis and progression of ILD often relies on high resolution computed tomography (HRCT) and pulmonary function tests (PFT). The goal of this study is to assess the agreement between functional and radiological changes longitudinally in patients with IIM-ILD.
Methods: This is a retrospective study on patients in the Northwell Myositis cohort. All patients met 2017 EULAR/ACR classification criteria for IIM. ILD diagnosis was identified by chart review and by presence of NSIP, COP/BOOP, UIP, and unspecified patterns on HRCT. We included 22 patients who had >2 corresponding HRCT and PFT, performed within 6 months of each other. Qualitative ILD patterns are reported using descriptive statistics.
Baseline FVC, FEV1, and DLCO values were collected, and percent changes were calculated for subsequent PFTs from baseline. Improvement or worsening was defined as ≥ 10% increase or decrease in 1 variable with no more than 5% decrease or increase in other variables. HRCT scans were categorized as improved, stable or worsened compared to the previous scan per radiologist assessment.
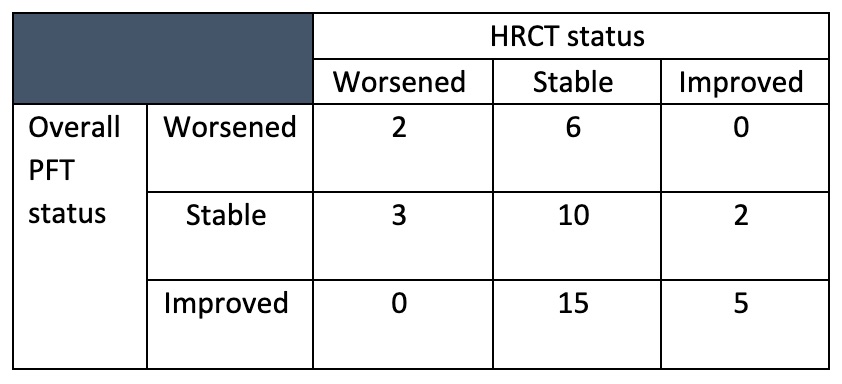
There were 65 matched HRCT/PFT pairs, ranging from 2 to 5 pairs per patient. Using initial HRCT and PFT as baseline, improvement, stability or worsening were assessed for 43 matched pairs using the above definition. Kappa statistics was calculated to measure the agreement between the changes seen on PFT versus HRCT.
Results: A total of 22 patients with median age of 57.5 years were included in the study. The average follow-up time was 5 years (range: 1-13years). The most common HRCT finding at baseline was bilateral groundglass opacities (77.3%, 17/22), followed by reticular opacities (36.4%, 8/22). The most common initial immunosuppressive agent in addition to steroid was mycophenolate mofetil (54.5%, 12/22), followed by methotrexate (18.2%, 4/22), azathioprine (9%, 2/22), and rituximab (9%, 2/22). Two patients received steroids alone and 1 patient declined treatment.
At baseline, mean FVC was 67% (SD:19. 3), mean FEV1 was 68.6% (SD:21.1), mean DLCO was 48.5% (SD:16.9). On PFT, 13.6% (3/22) patients worsened, 27.3% (6/22) were stable, and 59.1% (13/22) improved. On HRCT, 22.7% (5/22) patients worsened, 54.5% (12/22) were stable, 22.7% (5/22) improved.
Agreement of improvement, stability or worsening for the follow-up pairs of HRCT and PFT is shown in Table 1. Kappa coefficient between these pairs was 0.071 (SE = 0.102, 95% CI -0.129 to 0.272), indicating poor agreement. When analysis was performed by combining improved and stable in one category, the coefficient marginally increased to 0.192 (SE = 0.181, 95% CI -0.129 to 0.272)
Conclusion: When comparing the agreement of HRCT and PFT to assess change in ILD status over time in this study, we found that more patients showed improvement on PFT than HRCT. While PFT was more likely to detect improvement, HRCT was more likely to document stability. The poor agreement between functional and radiological changes demonstrated in this study suggested the deficiency in current methods for monitoring ILD progression. More sensitive modalities are needed to detect change over time in patients with immune-mediated ILD.
To cite this abstract in AMA style:
Narain S, Hu C, Liu M, Vashistha H, Shargani K, Marder G. Evaluation of Agreement Between Functional and Radiological Changes in Idiopathic Inflammatory Myositis (IIM) Associated Interstitial Lung Disease (ILD) [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/evaluation-of-agreement-between-functional-and-radiological-changes-in-idiopathic-inflammatory-myositis-iim-associated-interstitial-lung-disease-ild/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/evaluation-of-agreement-between-functional-and-radiological-changes-in-idiopathic-inflammatory-myositis-iim-associated-interstitial-lung-disease-ild/