Session Information
Date: Sunday, November 8, 2020
Title: T Cell Biology & Targets in Autoimmune & Inflammatory Disease Poster
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Antisynthetase syndrome (AS) is a systemic autoimmune disorder characterized by the presence of anti-aminoacyl-tRNA synthetase antibodies, myositis, interstitial lung disease (ILD), mechanics hands, and raynaud’s phenomenon. Dermatomyositis (DM) is a similar autoimmune disorder with clinical features of muscle weakness, ILD, neoplasms, gottron’s papules, and photosensitive cutaneous manifestations. Currently most clinicians see AS as a subclassification under DM due to the many similarities. Recently some studies have emerged identifying differences in the type I interferon system between AS and DM muscle and finger eruptions. Type I interferons are amplified in autoimmune diseases such as DM, as demonstrated by proteins such as MxA expression. To further characterize these differences, we investigated the cellular composition and inflammatory pathway profile using immunofluorescent staining (IF) and image mass cytometry (IMC).
Methods: We evaluated skin biopsies from back, arm, or leg of 7 DM patients, 3 AS patients, and 3 healthy control (HC). IF was performed on 3 biopsies from each group for IFNβ and MxA. Subsequently, IMC was implemented to further identify differences between DM and AS using metal conjugated antibodies. Biopsies were stained with a cocktail of markers and 1mm x 2mm regions were ablated using the Hyperion Imaging System. Cells were segmented using a nuclear app-based algorithm in Visiopharm. Per cell mean pixel intensity (MPI) analysis was performed using histoCAT. The Phenograph algorithm was used to cluster cells based on expression of cell type markers. The Kruskal Wallis test was used to identify immunofluorescence IFNβ and MxA differences between HC, DM, and AS groups corrected for multiple comparisons by controlling False Discovery Rate. The Mann Whitney test was used to identify differences in IMC cell populations and pathway expression between AS and DM skin lesions, including mDC IFNβ.
Results: IF of AS skin showed increased IFNβ and MxA compared to HC (p< 0.05, Fig 1) but there was no difference compared to DM IFNβ and MxA (p >0.05, Fig 1). IMC cell clusters in AS and DM were similarly distributed and we identified no differences in the cell populations (macrophages, T cells, and dendritic cells) of AS and DM (p >0.05, Fig 2). Despite no statistical differences in cells there is a trend for increased CD14+CD16+, mDCs, and pDCs in DM. Pathway expressions of pPPARγ, pSTING, IL31, IFNβ, MxA, pTBK1, IFNγ, and pERK also did not differ between AS and DM (p >0.05, Fig 3). The pIRF3, IL4, and IL17 pathways were increased in DM compared to AS skin lesion (p=0.04, 0.01, and 0.01, Fig 3). Both AS and DM mDCs produced IFNβ (Fig3), but there was no difference in mDC IFNβ between AS and DM (p >0.05, Fig 3).
Conclusion: A similar immune composition exists in AS and DM skin and there is a role for the type I interferon system in AS, however there may be differences in the extent of involvement due to decreased pIRF3,trends for decreased MxA, and dendritic cells. Additional differences in cytokines IL4 and IL17 exist with increased expression in DM. However, the two diseases overlap significantly supporting their current classification, but larger studies are still needed to clarify differences.
 Immunofluorescence staining of IFNβ and MxA in HC, DM, and ASA skin a-c) HC skin has little IFNβ (green, a) compared to DM skin (b) and ASA skin (c). e-f) HC skin also has decreased MxA (red, d) compared to DM skin (e) and ASA skin (f) with DAPI in blue (a-f). Quantification of mean fluorescence intensity shows increased IFNβ in DM and ASA lesional skin compared to HC (g) and increased MxA expression in DM and ASA lesional skin compared to HC (h). Nuclei represented by DAPI (blue, a-f) * p < 0.05
Immunofluorescence staining of IFNβ and MxA in HC, DM, and ASA skin a-c) HC skin has little IFNβ (green, a) compared to DM skin (b) and ASA skin (c). e-f) HC skin also has decreased MxA (red, d) compared to DM skin (e) and ASA skin (f) with DAPI in blue (a-f). Quantification of mean fluorescence intensity shows increased IFNβ in DM and ASA lesional skin compared to HC (g) and increased MxA expression in DM and ASA lesional skin compared to HC (h). Nuclei represented by DAPI (blue, a-f) * p < 0.05
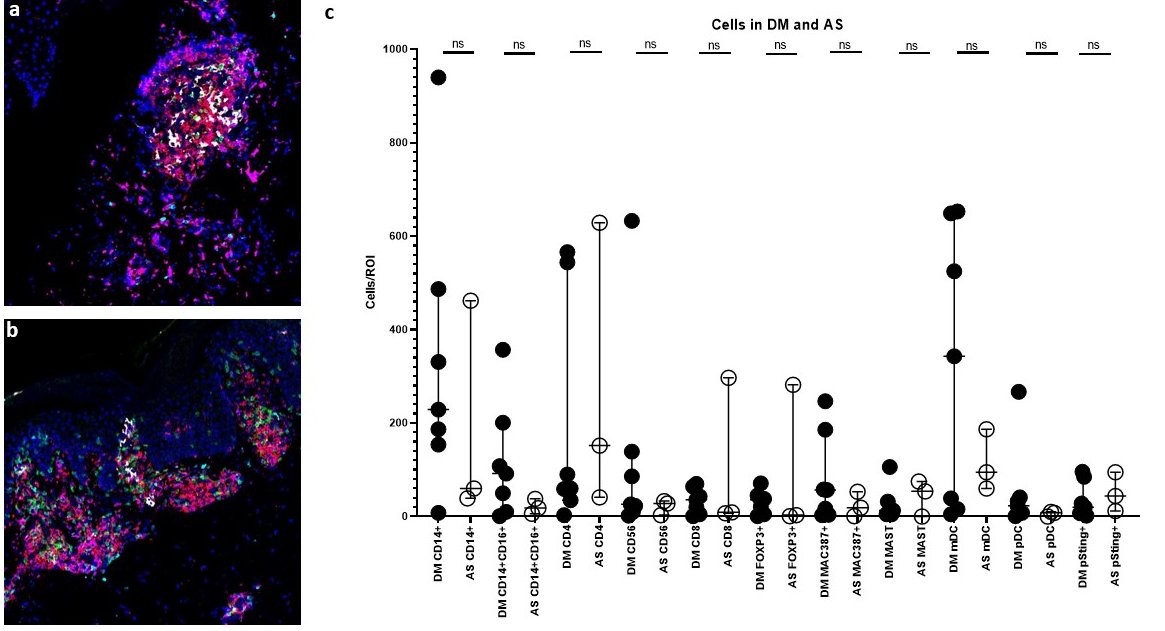 Immune Cell quantification between HC, DM, and AS patients using Image Mass Cytometry PhenoGraph populations. a-b) Multiplexed image of lesional DM(a) and AS(b) skin revealing similar cells CD4 (red), CD8(green), DNA (blue), CD11C+ (white), BDCA1+ (cyan), and CD14+ (magenta) cells. c) The cell counts of CD14+, CD14+CD16+, MAC387+, CD4+, FOXP3+, Mast, CD56+, pSTING+CD14+CD16+, mDC, pDC, and CD8 were compared between DM and AS skin lesions. No significant differences were found between DM and AS for all cell populations.
Immune Cell quantification between HC, DM, and AS patients using Image Mass Cytometry PhenoGraph populations. a-b) Multiplexed image of lesional DM(a) and AS(b) skin revealing similar cells CD4 (red), CD8(green), DNA (blue), CD11C+ (white), BDCA1+ (cyan), and CD14+ (magenta) cells. c) The cell counts of CD14+, CD14+CD16+, MAC387+, CD4+, FOXP3+, Mast, CD56+, pSTING+CD14+CD16+, mDC, pDC, and CD8 were compared between DM and AS skin lesions. No significant differences were found between DM and AS for all cell populations.
 Mean Pathway Expression in skin lesions of DM and ASA patients a) The mean expression per cell of pathways pPPARγ, pSTING, IL31, IFNβ, pRF3, pTBK1, IFNγ, IL4, IL17, and pERK was compared between AS and DM skin lesions. No significant differences between DM and AS were observed for pPPARγ, pSTING, IL31, IFNβ, pTBK1, IFNγ, and pERK. DM skin had increased expression of pIRF3, IL4, and IL17. b-g) DM and AS mDCs express IFNβ. CD11C mDCs (red, b,e) overlap with IFNβ (green, c,f) as seen in yellow (d,g). Individual mDCs overlapping with IFNβ are highlighted with white arrows. Nuclei represented with Ir-Intercalator (blue, b-g). Scale bars (gray) = 50μm h) DM and AS mDCs do not differ in mean IFNβ expression at a single cell level. * p < 0.05, ** p < 0.01,
Mean Pathway Expression in skin lesions of DM and ASA patients a) The mean expression per cell of pathways pPPARγ, pSTING, IL31, IFNβ, pRF3, pTBK1, IFNγ, IL4, IL17, and pERK was compared between AS and DM skin lesions. No significant differences between DM and AS were observed for pPPARγ, pSTING, IL31, IFNβ, pTBK1, IFNγ, and pERK. DM skin had increased expression of pIRF3, IL4, and IL17. b-g) DM and AS mDCs express IFNβ. CD11C mDCs (red, b,e) overlap with IFNβ (green, c,f) as seen in yellow (d,g). Individual mDCs overlapping with IFNβ are highlighted with white arrows. Nuclei represented with Ir-Intercalator (blue, b-g). Scale bars (gray) = 50μm h) DM and AS mDCs do not differ in mean IFNβ expression at a single cell level. * p < 0.05, ** p < 0.01,
To cite this abstract in AMA style:
Patel J, Ravishankar A, Maddukuri S, Bax C, Werth V. Evaluating the Cellular Composition of Anti-synthetase Syndrome and Dermatomyositis Skin Lesions Using Image Mass Cytometry [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/evaluating-the-cellular-composition-of-anti-synthetase-syndrome-and-dermatomyositis-skin-lesions-using-image-mass-cytometry/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/evaluating-the-cellular-composition-of-anti-synthetase-syndrome-and-dermatomyositis-skin-lesions-using-image-mass-cytometry/
