Session Information
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: No-show visits in various clinical settings are costly to providers and to health care systems, potentially representing between 3-14% of a clinic’s yearly income. This revenue challenge is compounded in rheumatology, as barriers to care delivery include socioeconomic factors for patients and prolonged wait times for appointments due to a growing shortage of rheumatologists nationwide. If patients at high risk for missing a referral appointment can be prospectively identified, then a strategic intervention to reduce the likelihood of a missed appointment will be fiscally advantageous and more effectively deliver rheumatic disease care to those in need. This study aims to characterize “no show” patients referred for outpatient rheumatology evaluation so that such a strategic intervention ultimately can follow.
Methods: Our electronic health record was queried for all patients who received ambulatory care referrals to a rheumatology provider within our healthcare system from January to December 2019. Basic demographic information, appointment characteristics and appointment outcomes were collected. Two patient groups were created based on their appointment outcomes; the first was comprised of all referred patients that no-showed, and the second included cancellations and completions. Patient and appointment characteristics were then compared between groups. Descriptive data is presented as mean (standard deviation) or median (interquartile range) for continuous variables and frequency (percentage) for categorical variables. Continuous variables were compared using a t-test or Mann-Whitney U test, as appropriate. Categorical data were analyzed using a chi-squared test or Fisher’s exact test, as appropriate. A multivariable regression model finally was constructed to determine odds of no-show using those variables that statistically differed between groups.
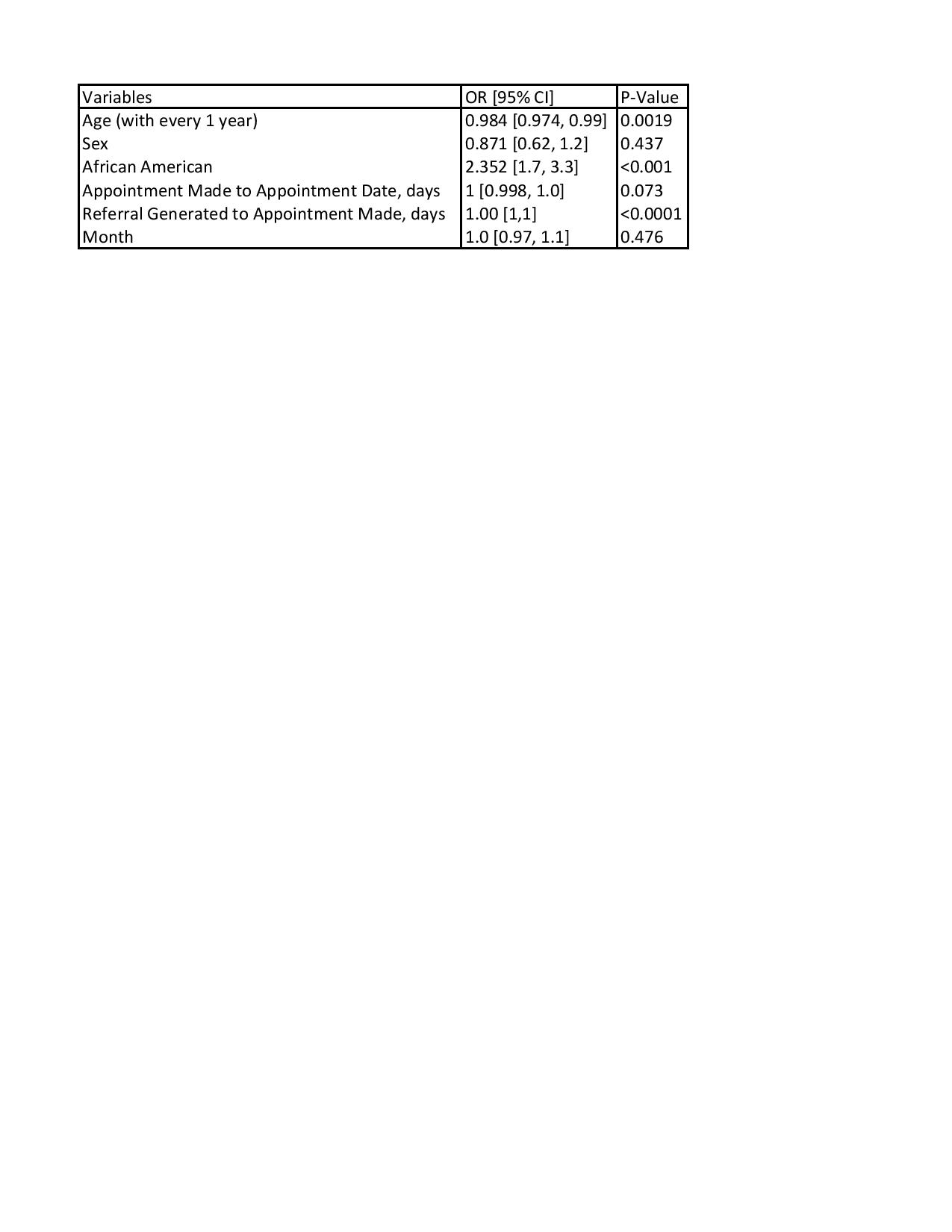
Results: Across Allegheny Health Network, 2167 unique patients received ambulatory referrals to rheumatology in 2019 [Table 1]; 186 were no-shows. The month of the appointment nor the time between the date the appointment was made and the actual appointment date reached significance in regards to higher risk of no showing, although November did have the highest rates (12% vs. 8.2%, p=0.09) [Table 2]. In multivariable analysis, younger age (50.7 y vs 53.7 y, p=0.009) and African American race (24% vs. 9.15%, p < 0.0001) increased the odds of no-showing to an appointment [Table 3]. Longer duration from when the referral was generated by the physician to when the patient called to make the appointment was noted in the group of patients that no showed (33.4 days vs 9 days, p=0.0002) [Table 2].
Conclusion: Demographic (younger age, African American race) and appointment features (delay in patients calling for an appointment) characterized practitioner-referred rheumatology patients at high risk for no-showing for a new patient appointment. Future strategies to reduce no-show rates should address socioeconomic barriers to health care in high-risk individuals and improve access to new patient appointments.
To cite this abstract in AMA style:
Bhatty O, Schorr R, Sharma T, Wasko M. Evaluating Patient No Show Rates to Rheumatology Appointments Across a Regional Healthcare System [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/evaluating-patient-no-show-rates-to-rheumatology-appointments-across-a-regional-healthcare-system/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/evaluating-patient-no-show-rates-to-rheumatology-appointments-across-a-regional-healthcare-system/