Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic lupus erythematosus (SLE) pregnancy is associated with a heightened risk of adverse pregnancy outcomes, including preeclampsia. Distinguishing preeclampsia from lupus nephritis (LN) presents a diagnostic conundrum due to overlapping signs and symptoms. Furthermore, the treatment approach differs significantly, with early delivery often indicated for the former, while additional immunosuppression is typical for the latter. To address this challenge, we aimed to elucidate the decision-making dynamics of healthcare specialists, specifically obstetricians/gynecologists (OBGYNs), rheumatologists, and nephrologists, regarding multiple SLE pregnancy scenarios.
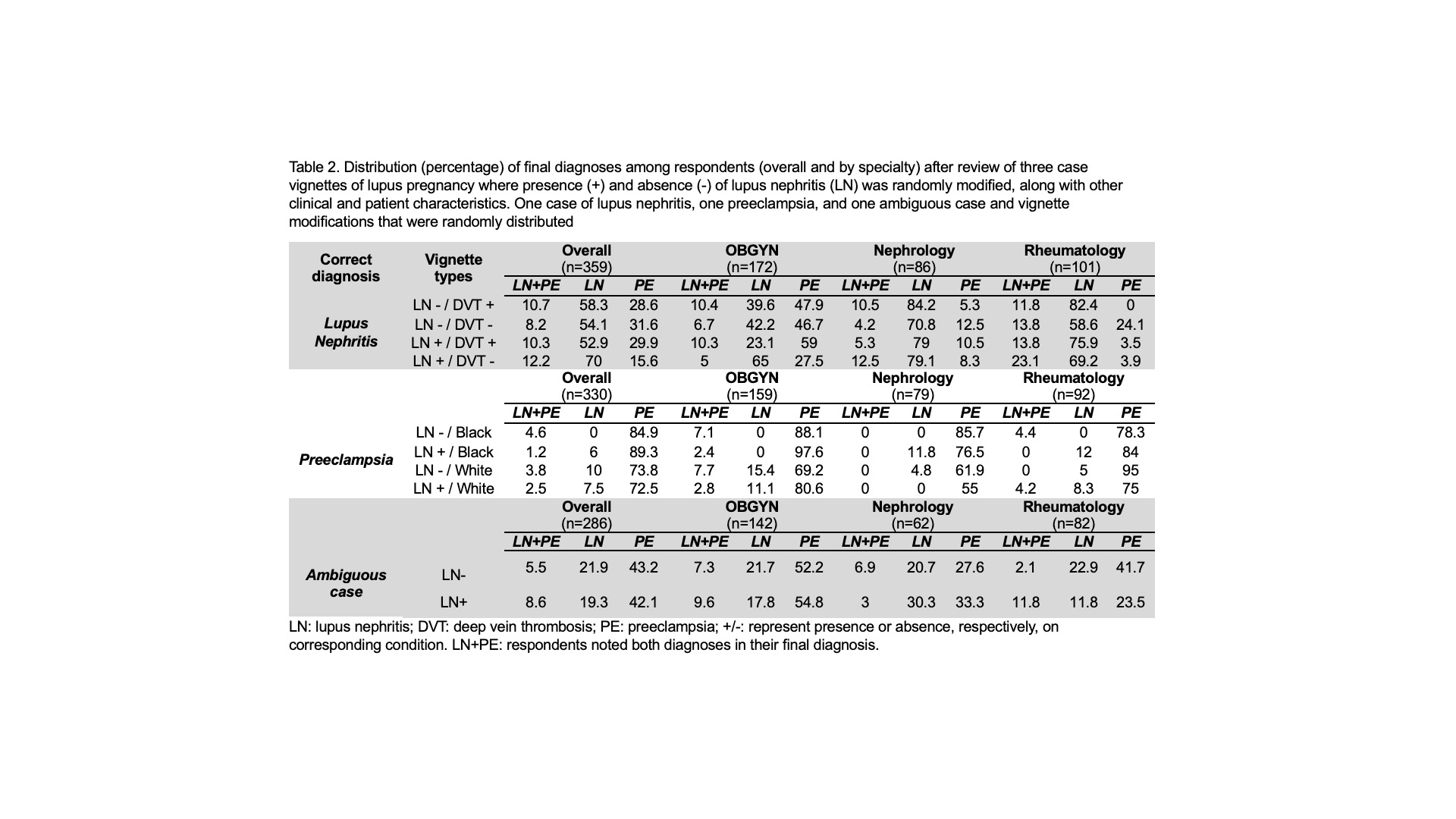
Methods: We designed clinical vignettes of 5 SLE pregnancies to simulate real-world scenarios. Within each vignette, we coded the instrument to randomly modify up to two features upon presentation (e.g., history of LN) to assess diagnostic inclinations. These case vignettes were included in a survey distributed to OBGYNs, rheumatologists, and nephrologists in the United States, yielding 359 respondents who provided demographic information and completed at least one vignette. This study compares diagnostic responses across medical specialties and vignette types—specifically LN, preeclampsia, and an ambiguous case—to examine how a history of LN influences diagnostic decisions. Statistical analysis included descriptive summaries of respondent characteristics, proportions of specified diagnoses by vignette type and specialty, and frequencies of write-ins for next diagnostic or therapeutic action and degree of certainty.
Results: Participants showed varying accuracy in diagnosing LN and preeclampsia across three vignettes in the presence and absence of LN history and additional modified characteristics. Nephrologists (70.8-84.2%), followed by rheumatologists (58.6-82.4%), were most likely to correctly diagnose LN, regardless of which variables were modified (Table 2). When diagnosing preeclampsia, OBGYNs displayed the highest proficiency (69.2-97.6%), followed by rheumatologists (75-95%). Regardless of the final diagnosis accuracy, most therapeutic and diagnostic next- step recommendations were consistent with those typically advised for LN or preeclampsia, with modest confidence levels overall.
Conclusion: Diagnostic decision-making dynamics among specialty physicians when dealing with LN and preeclampsia during SLE pregnancies are incompletely understood. Using a novel vignette-based approach, we identified specialist-specific diagnostic tendencies that provide insights into this important issue. By investigating these distinctions, we hope to encourage an even greater multidisciplinary approach to this clinical conundrum and ultimately improve patient care.
To cite this abstract in AMA style:
Stolyar L, Sediqi S, Lafayette R, Druzin M, Hawa S, Moyer A, Chaichian Y, Simard J. Evaluating Clinical Reasoning in Randomized Surveys of Lupus Nephritis and Preeclampsia Pregnancy Case Workups: A Clinical Conundrum [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/evaluating-clinical-reasoning-in-randomized-surveys-of-lupus-nephritis-and-preeclampsia-pregnancy-case-workups-a-clinical-conundrum/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/evaluating-clinical-reasoning-in-randomized-surveys-of-lupus-nephritis-and-preeclampsia-pregnancy-case-workups-a-clinical-conundrum/