Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Prior work has shown that Scl-70 positive autoantibody status and baseline c-reactive protein (CRP) are associated with more rapid pulmonary function decline in patients with systemic sclerosis (SSc). We previously found that patients with esophageal dilation on chest high-resolution computer tomography (HRCT) scan had lower % predicted forced vital capacity (FVC) and diffusing capacity for carbon monoxide (DLCO) at baseline. The purpose of this study is to identify clinical factors, including HRCT esophageal dilation, that are associated with pulmonary function decline in SSc.
Methods: Included participants were enrolled in the Northwestern Scleroderma Registry, fulfilled 2013 SSc criteria, and had ≥1 HRCT and ≥2 pulmonary function tests (PFT) obtained as standard of care. The widest esophageal diameter (WED) and radiographic interstitial lung disease (ILD) were assessed using published methods. The WED was dichotomized as dilated (≥19 mm) vs. not dilated (< 19mm) based upon published data. Clinically meaningful PFT change was defined as % predicted FVC ≥5-point difference and % predicted DLCO ≥15-point difference based upon published data. Clinical characteristics at the time of baseline HRCT scan were collected. Pulmonary arterial hypertension (PAH) was present if mean pulmonary arterial pressure was ≥25 mmHg on right heart catheterization. Linear mixed effect models were used to model PFT change.
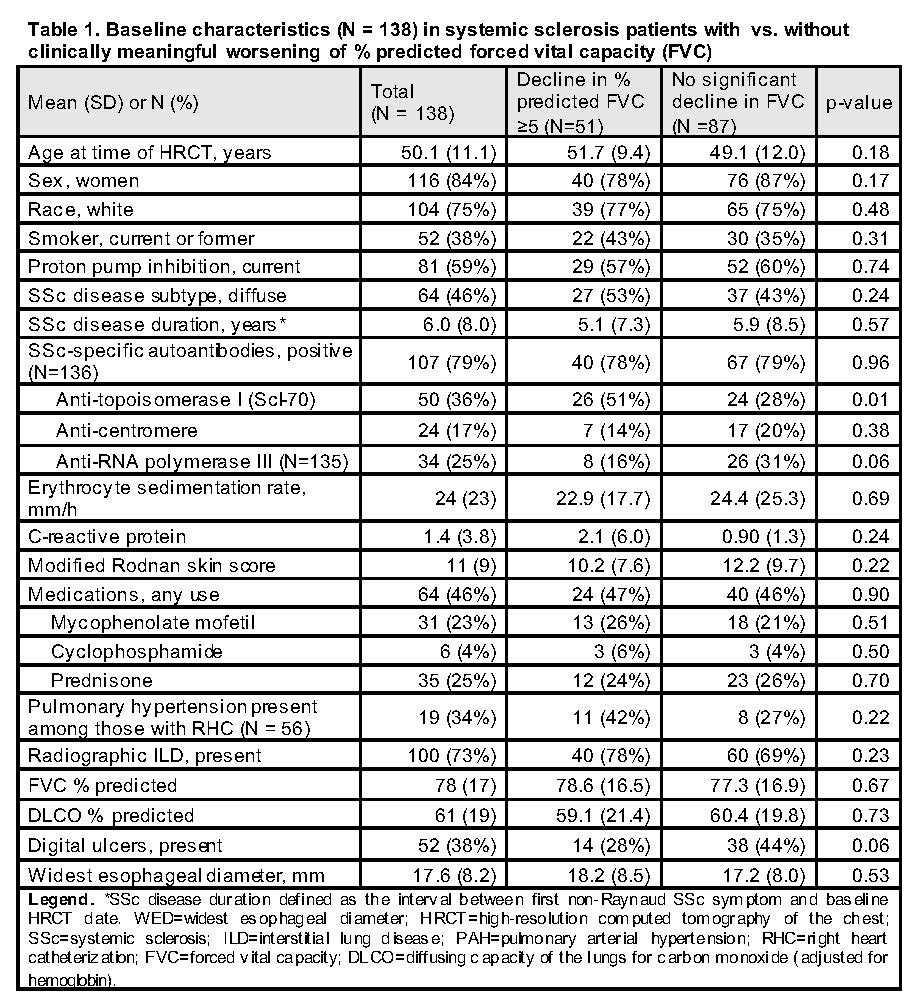
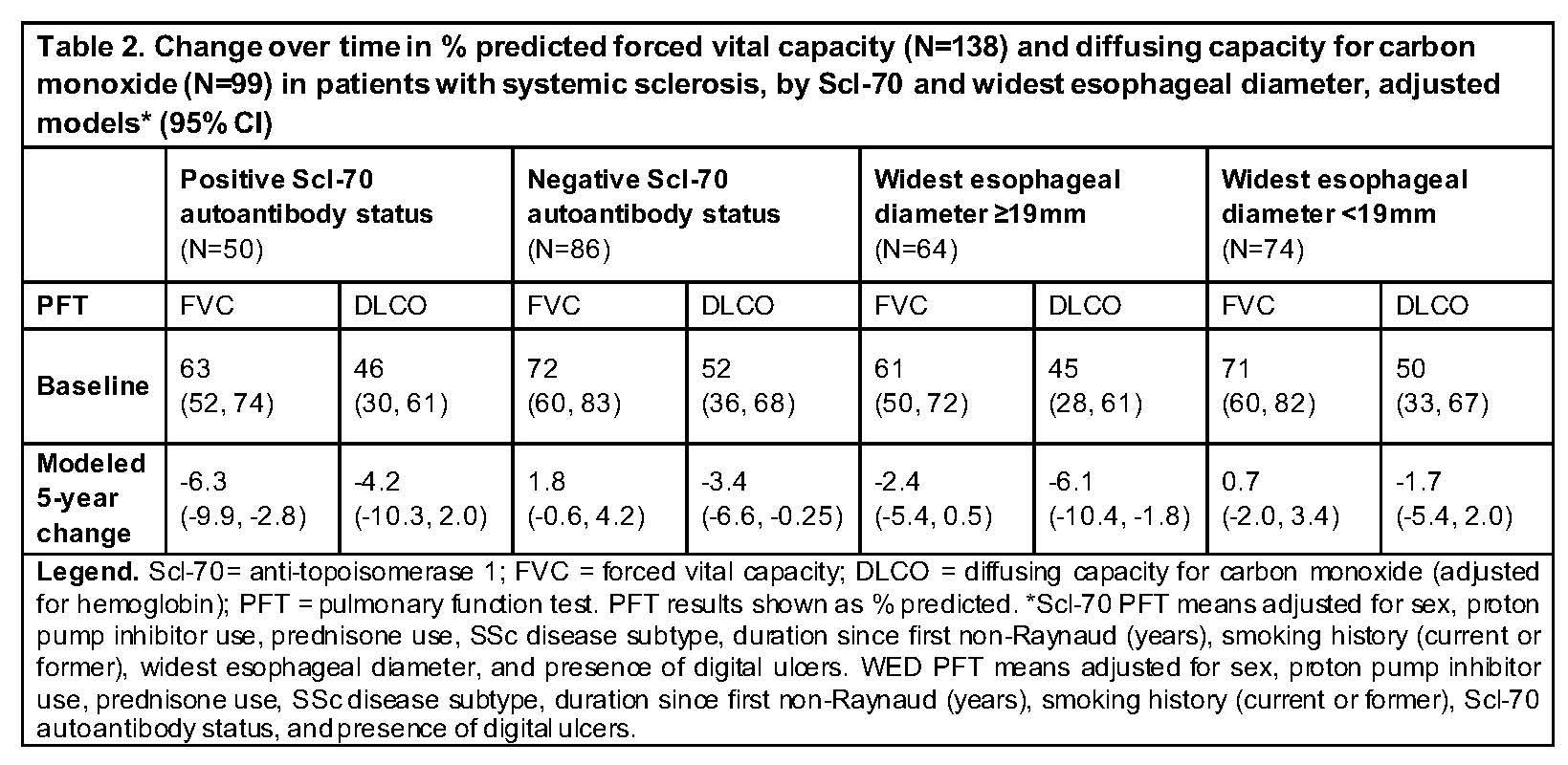
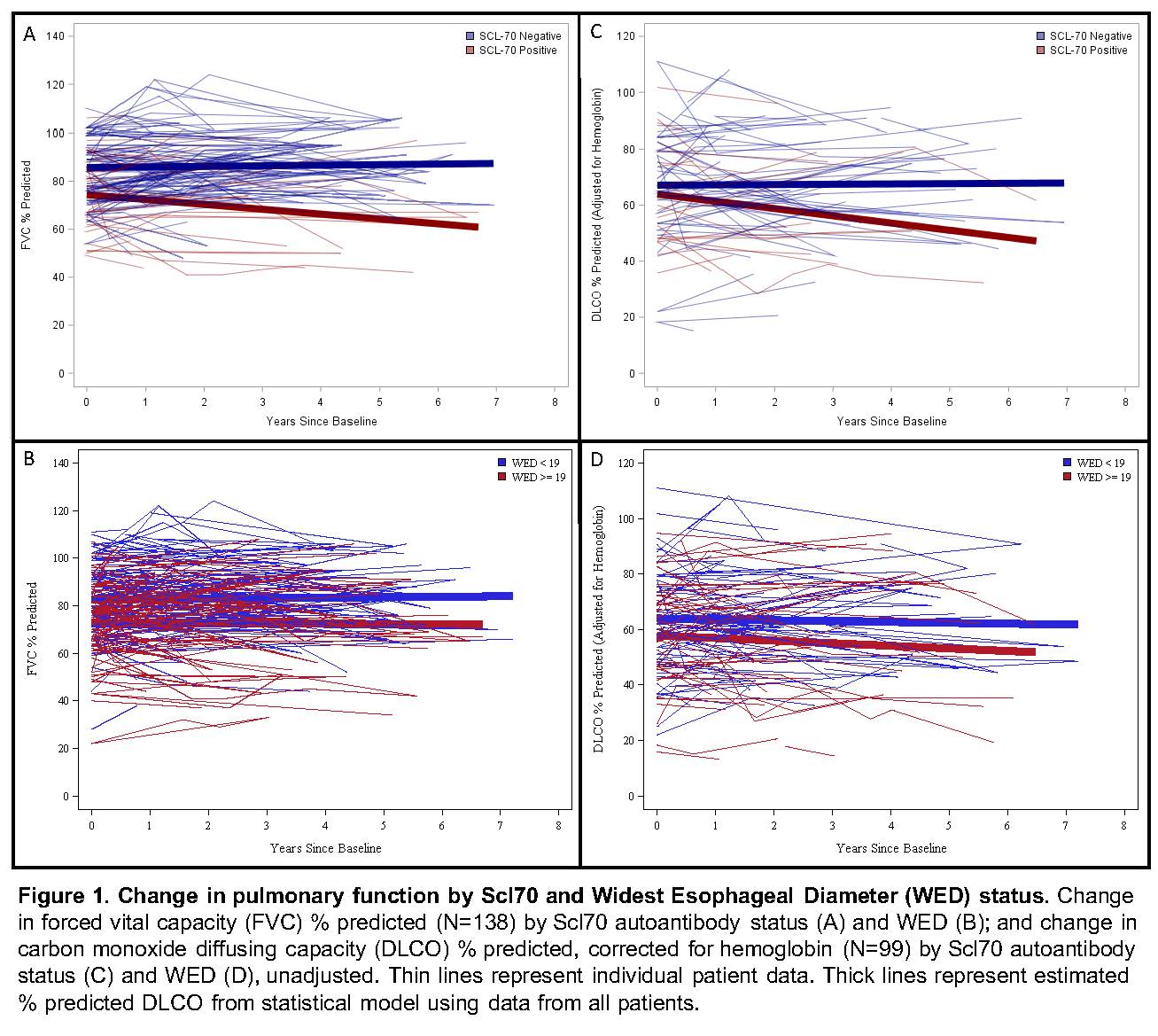
Results: 138 SSc patients met study criteria. Radiographic ILD was present in 100 of 138 (73%) participants (Table 1). 51 of 138 (40%) patients demonstrated clinically meaningful FVC decline (median follow-up 2.8 years). In adjusted models, patients with (vs. without) esophageal dilation had statistically significant 5-year % predicted DLCO decline (-6.1; 95% CI -10.4, -1.8), however this change did not meet the 15-percentage point threshold for clinical significance (Table 2, Figure 1). There was no difference in the presence of PAH at baseline between those with vs. without DLCO decline (14% vs. 13%, p=0.51). Patients with positive (vs. negative) Scl-70 autoantibody status had statistically significant 5-year % predicted FVC decline (-6.3; 95% CI -9.9, -2.8) (Table 2, Figure 1). Esophageal diameter did not distinguish between those with vs. without significant FVC decline. There was no difference in baseline SSc disease duration, modified Rodnan skin score, smoking status, gender, age, baseline CRP, or race between those with vs. without clinically meaningful FVC change.
Conclusion: Scl-70 positivity, but not elevated baseline CRP, is a risk factor for % predicted FVC decline. Esophageal dilation on HRCT was associated with a minimal, non-clinically significant 5-year decline in DLCO and no change in FVC during follow-up. These results have important prognostic implications for SSc-ILD patients with esophageal dilation.
To cite this abstract in AMA style:
Showalter K, Hoffmann A, Richardson C, Koloms K, Rouleau G, Aaby D, Lee J, Dematte J, Agrawal R, Wu X, Chang R, Hinchcliff M. Esophageal Dilation and Other Clinical Factors Associated with Pulmonary Function Decline in Patients with Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/esophageal-dilation-and-other-clinical-factors-associated-with-pulmonary-function-decline-in-patients-with-systemic-sclerosis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/esophageal-dilation-and-other-clinical-factors-associated-with-pulmonary-function-decline-in-patients-with-systemic-sclerosis/