Session Information
Date: Tuesday, November 10, 2015
Title: Systemic Lupus Erythematosus - Clinical Aspects and Treatment Poster Session III
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Hematuria in lupus nephritis (LN) is secondary
to the passage of red blood cells (RBCs) through glomerular abnormalities. Dysmorphic RBCs are associated with glomerulonephritis, and
particularly the acanthocytes that are the typical dysmorphic-glomerular RBCs. Kidney biopsy (KB) in
LN–that informs the activity (Austin et al1.), and the LN
class– is helpful guiding treatment and prognosis. Objectives: To evaluate
the correlation between the activity (in KB) and the count of total RBCs/acanthocytes in urine of patients with LN. Secondary
objective was to assess if the count of RBCs, and the percentage of acanthocytes discriminate among the LN classes.
Methods: Patients with LN undergoing KB were
invited to participate in our study. The morning before the KB, a urine sample
was obtained and evaluated (after centrifugation) for the number of RBCs in a Neubauer chamber; the percentage of acanthocytes
was also determined. KBs were evaluated by a nephro-pathologist
who evaluated the class and activity of LN (0-24 points for proliferative
classes); non-proliferative forms of LN were assigned as 0 of activity. Correlation
was evaluated with Spearman’s rho and median difference with Mann-Whitney’s U. A
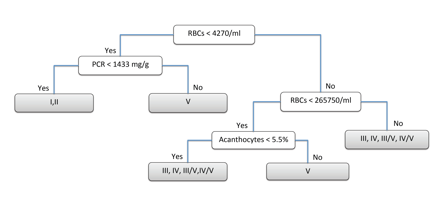
classification tree was performed to distinguish between proliferative (III,
IV, III/V, IV/V), pure membranous (V) or other classes of LN (I,II). Statistical analysis was performed using R version
3.2.0.
Results: We included
39 patients, 28 women (71.8%); three patients (7.7%) had LN class I, 3 (7.7%)
class II, 5 (12.8%) class III, 13 (33.3%) class IV, 11 (28.2%) class V, 3
(7.7%) class III/V and 1 (2.6%) class IV/V. The median activity of LN was 4
(0-18). The RBCs count had a positive correlation with the LN activity
(r=0.7058, p<0.0001); the number of acanthocytes
had also a positive correlation with activity of LN (r= 0.6460, p<0.0001). Patients
with proliferative LN had higher count of RBCs than non-proliferative LN
(434,000 vs 29,000, p<0.001) and higher total
count of acanthocytes (27,350 vs 2,860,
p= 0.0005). The classification tree (Figure 1) shows that RBCs, the protein/creatinine ratio (PCR), and the acanthocytes
percentage can be helpful for predicting LN class; the misclassification error
rate of this tree was 17.95%.
Conclusion: Evaluation
of urine abnormalities is a window of LN histopathology, particularly RBCs, acanthocytes, and PCR.
References
1. Austin HA, et al. Kidney Int.
1984;25(4):689–95.
Figure 1. Classification tree for predicting class of LN.
To cite this abstract in AMA style:
Martinez-Martinez MU, Llamazares-Azuara L, Martínez-Galla D, Valadez-Castillo F, Mandeville P, Borjas García JA, Abud-Mendoza C. Erythrocytes, Acanthocytes, and Proteins in Urine Reflect Lupus Nephritis Histology [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/erythrocytes-acanthocytes-and-proteins-in-urine-reflect-lupus-nephritis-histology/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/erythrocytes-acanthocytes-and-proteins-in-urine-reflect-lupus-nephritis-histology/