Session Information
Date: Sunday, November 8, 2020
Title: Epidemiology & Public Health Poster III: Inflammatory Rheumatic Disease
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Individuals with systemic lupus erythematosus (SLE) have multiple risk factors for upper gastrointestinal bleeding (UGIB), including heightened susceptibility to infection and glucocorticoid, NSAID and anticoagulant use. We aimed to examine the epidemiology and sociodemographic distribution of UGIB in a population-based SLE cohort enrolled in Medicaid, the largest U.S. insurance for low income individuals.
Methods: Using Medicaid claims data from 47 states (2000-2006) and from 29 states (2007-2010), we identified individuals 18-65 years with SLE (≥3 ICD-9 codes of 710.0 ≥30 days apart), with ≥12 months of continuous enrollment (baseline period) prior to the third SLE code (index date). Our outcome was UGIB (ED visit or hospitalization discharge diagnosis codes beginning the day following the index date). We assessed demographic factors, medication use, and comorbidities during the 12-month baseline period prior to and including the index date and determined the incidence rates (IR, 95% CI) of UGIB overall and by sociodemographics, medications and comorbidities. We used Cox regression models to compare risk (HR, 95% CI) of first UGIB by these factors. We age, sex and index date-matched SLE patients to the general Medicaid population (1:4, 2007-2010) and compared the HRs of UGIB adjusted for sociodemographic factors, medications and comorbidities. In sensitivity analyses we excluded individuals with UGIB during the baseline period.
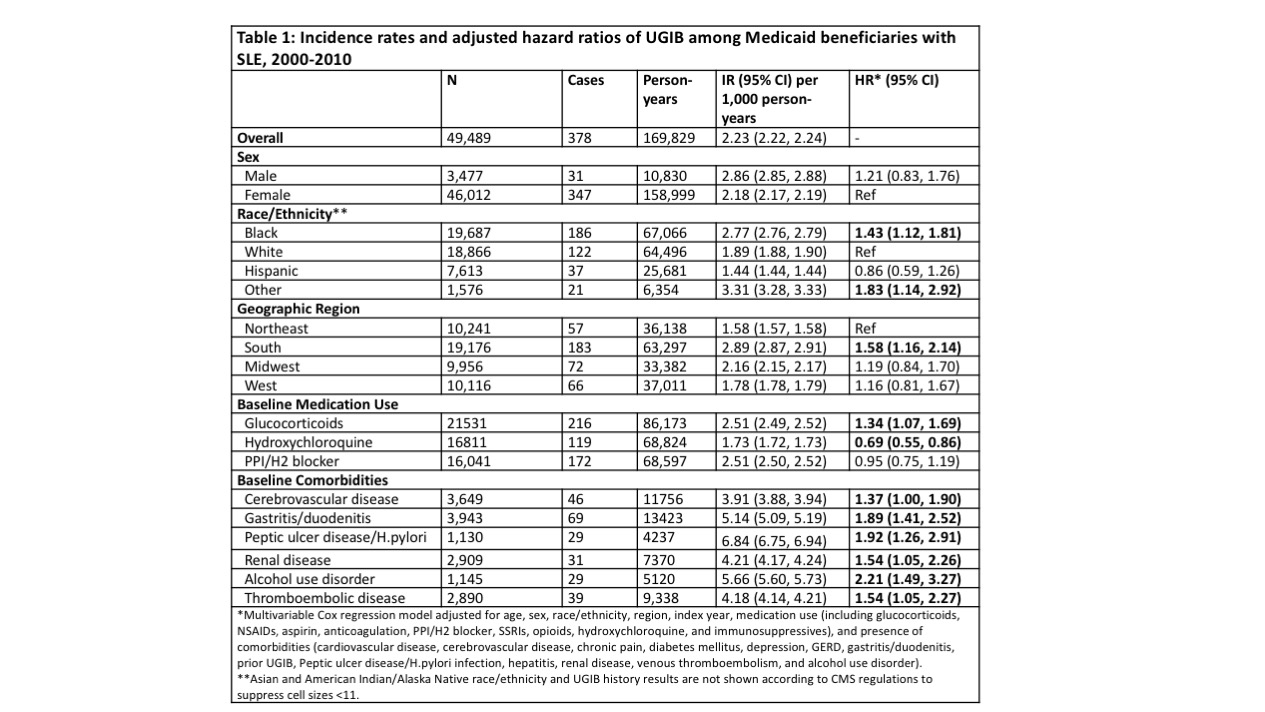
Results: Among 49,489 Medicaid beneficiaries with SLE, the mean (SD) age was 42.2 (11.7) years, 93% were female, 40% black, 38% white, 15% Hispanic, and 39% were from the South. The mean (SD) follow-up was 3.4 (3) years. There were 378 ED visits or hospitalizations for UGIB (IR 2.23/1000 person-years) (Table 1). In adjusted models, the risk of UGIB was higher among blacks compared to whites (HR 1.43, 95% CI 1.12-1.81), and in the South compared to the Northeast (HR 1.58, 95% CI 1.16-2.14). Baseline UGIB, cerebrovascular disease, gastritis/duodenitis, peptic ulcer disease/H.pylori infection, renal disease, alcohol use disorder, and glucocorticoid use were associated with higher risk, while hydroxychloroquine was associated with lower risk (HR 0.69, 95% CI 0.55-0.86). Proton pump inhibitors (PPIs) and H2 blockers were not associated with lower UGIB risk (HR 0.95, 95% CI 0.75-1.19). In medication and comorbidity-adjusted age and sex matched analyses (2007-2010), individuals with SLE had 4.28 times higher risk of UGIB (95% CI 2.39-7.68) compared to the general Medicaid population. After excluding patients with UGIB at baseline, IRs and risk factors were similar.
Conclusion: Among Medicaid beneficiaries, individuals with SLE had >4 times higher risk of UGIB compared to the general population. Black race, residence in the South, related comorbidities and glucocorticoid use were associated with higher risk. Baseline hydroxychloroquine use was associated with reduced risk of UGIB, perhaps a marker of higher quality care, while PPIs and H2 blockers were not, likely because they were prescribed to higher risk individuals. Further studies are needed to understand the efficacy of prevention strategies given this significant burden of UGIB among individuals with SLE.
To cite this abstract in AMA style:
Xu C, Perencevich M, Kim S, Costenbader K, Feldman C. Epidemiology and Sociodemographic Distribution of Upper Gastrointestinal Bleeding Among Medicaid Beneficiaries with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/epidemiology-and-sociodemographic-distribution-of-upper-gastrointestinal-bleeding-among-medicaid-beneficiaries-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/epidemiology-and-sociodemographic-distribution-of-upper-gastrointestinal-bleeding-among-medicaid-beneficiaries-with-systemic-lupus-erythematosus/