Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: A previous survey of Australian Rheumatologists indicated low confidence (60% of Australian Rheumatologists) in the use of Temporal artery ultrasound provided by their Radiology services in the diagnosis of giant cell arteritis. There is limited published information on multimodal imaging to enhance diagnostic confidence of GCA. The aim of this study was to determine the utility of standardized high-resolution temporal artery scanning protocols for diagnosis of GCA and the role of multimodal imaging in increasing the confidence of GCA diagnosis.
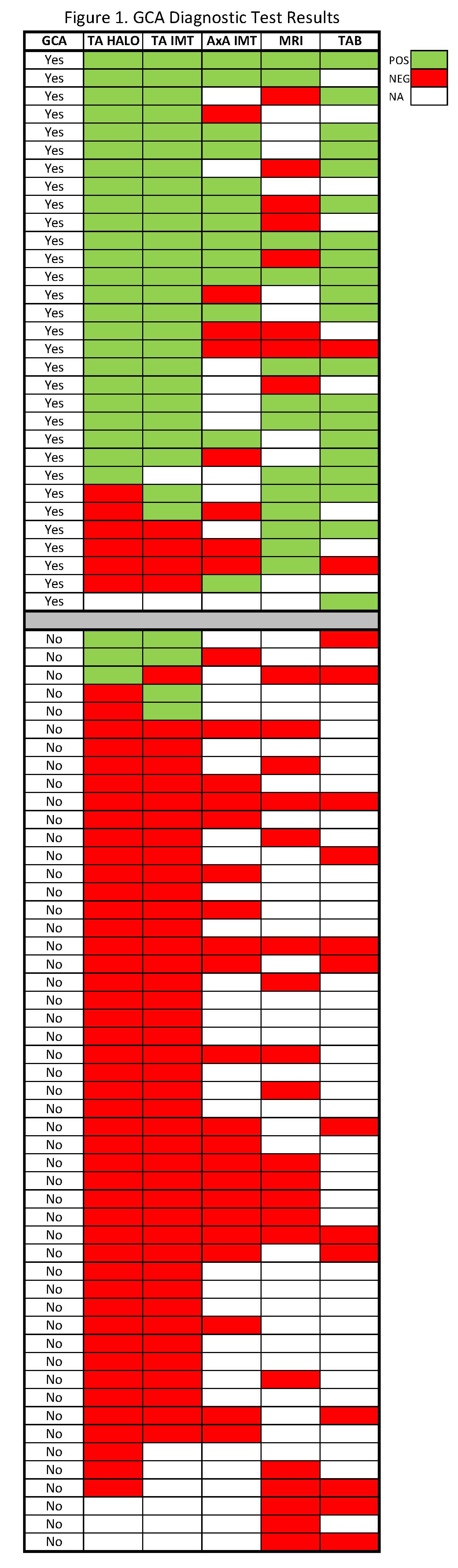
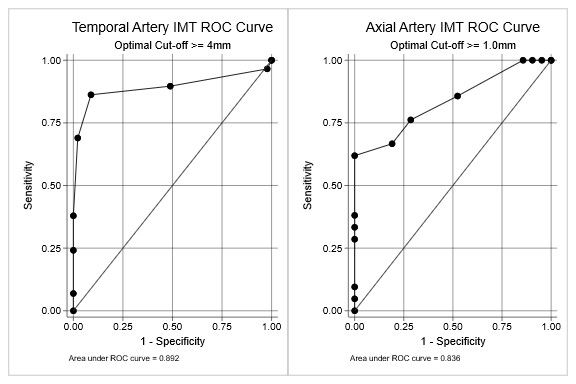
Methods: Consecutive patients from 2020 to 2022 with suspected GCA based on 3/5 1990 ACR classification criteria were enrolled. Patients underwent ultrasound of bilateral common superficial temporal arteries (CSTA) and main branches with a 22MHz linear ultrasound probe to determine the arterial intima-media thickness (IMT) at the CSTA and the presence of a non-compressible halo on color Doppler.Bilateral axillary artery (AA) IMT was measured in some patients. Additional diagnostic tests included dedicated 3Tesla MRI of scalp arteries time of flight sequence with grading of gadolinium enhancement of temporal artery (TA) wall and temporal artery biopsy (TAB) or 18FDG PET scan. Final diagnosis of GCA was determined at case-note review at 6 months by consultant rheumatologist. At least two diagnostic tests were performed on most patients. GCA diagnostic confidence was enhanced by employing multimodality imaging and biopsy. Optimal IMT cut-off measurements for GCA diagnosis were determined by Receiver Operating Characteristic analysis.
Results: 82 patients were included in the study (mean age 72 years, 66% female). Mean age was higher in the 31 (38%) patients with confirmed GCA diagnosis than those without GCA confirmation (79 vs 68 years, p=0.0002).
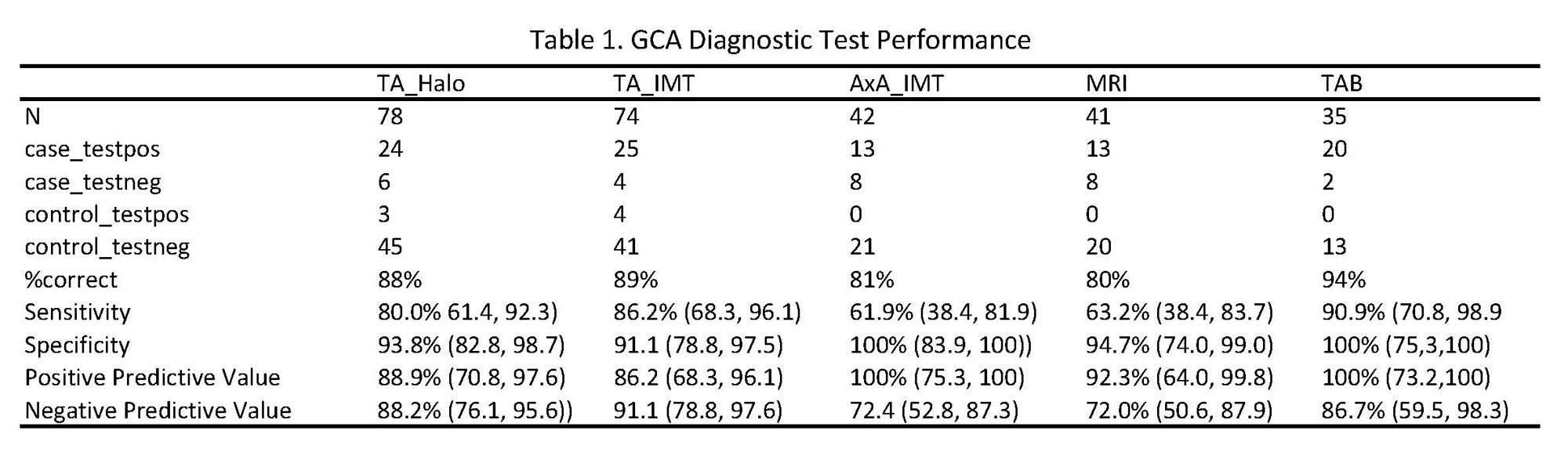
Of the 82 patients, 78 (95%) underwent ultrasound, 41 MRI (50%), 15 PET (18%) and 35 TAB (43%). 71% had at least two diagnostic procedures and 33% had three. The optimal IMT cut-off measurements were 0.4mm for CSTA (n=74, 86% sensitivity, 91% specificity) and 1mm for AA (n=42, 62% sensitivity,100% specificity). Sensitivity and specificity of TA halo for GCA (n=78) was 80% and 94% respectively and 63% and 95% respectively for Grade 2 Gadolinium enhancement of TA (n=41).
Conclusion: High resolution ultrasound TA Halo, and the more objective TA IMT, both performed well for cranial GCA diagnosis with excellent sensitivity and specificity.
To cite this abstract in AMA style:
Ninan J, Lyne S, McNeil J, Tieu J, Limaye V, Proudman S, Lester S, Hill C. Enhanced Diagnostic Confidence with High Frequency Temporal Artery Ultrasound in Diagnosis of Cranial Giant Cell Arteritis (GCA) [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/enhanced-diagnostic-confidence-with-high-frequency-temporal-artery-ultrasound-in-diagnosis-of-cranial-giant-cell-arteritis-gca/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/enhanced-diagnostic-confidence-with-high-frequency-temporal-artery-ultrasound-in-diagnosis-of-cranial-giant-cell-arteritis-gca/