Session Information
Date: Tuesday, October 23, 2018
Title: Systemic Lupus Erythematosus – Clinical Poster III: Treatment
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Musculoskeletal (MS) pain is a common symptom of patients with Systemic Lupus Erythematosus (SLE) affecting up to 95% of patients and contributing to a reduced quality of life. Safe and efficacious treatment remains an unmet need for this disease feature. The cholinergic anti-inflammatory pathway is a physiologic mechanism diminishing inflammation. Stimulation of the vagus nerve results in reduction of inflammatory mediators with beneficial effects in both human inflammation and animal models of disease. We proposed to evaluate transcutaneous, noninvasive stimulation of the vagus nerve through its auricular branch in SLE patients with MS pain.
18 SLE patients with MS pain ≥ 4 on an anchored 10cm Visual Analog Scale for pain and MS activity defined by SLEDAI-2K arthritis or a BILAG MS score ≥ C, were randomized (2:1) in this double-blind study to receive 5 minutes of transcutaneous auricular vagus nerve or sham stimulation (taVNS or SS) for 4 consecutive days. Patients with a diagnosis of fibromyalgia were excluded. For sham stimulation, electrodes were placed on the earlobe and no current was delivered. Evaluations at baseline, day 5 and day 12 included patient assessments of pain, disease activity (PtGA) and fatigue. Tender and swollen joints, SLEDAI-2K and the Physician Global Assessment (PGA) were completed by a blinded physician. Potential biomarkers were also determined at these times and included serum levels of acute phase reactants, inflammatory cytokines as well as cytokine levels following whole blood stimulation (WBS) with TLR 4, 7 or 9 agonists.
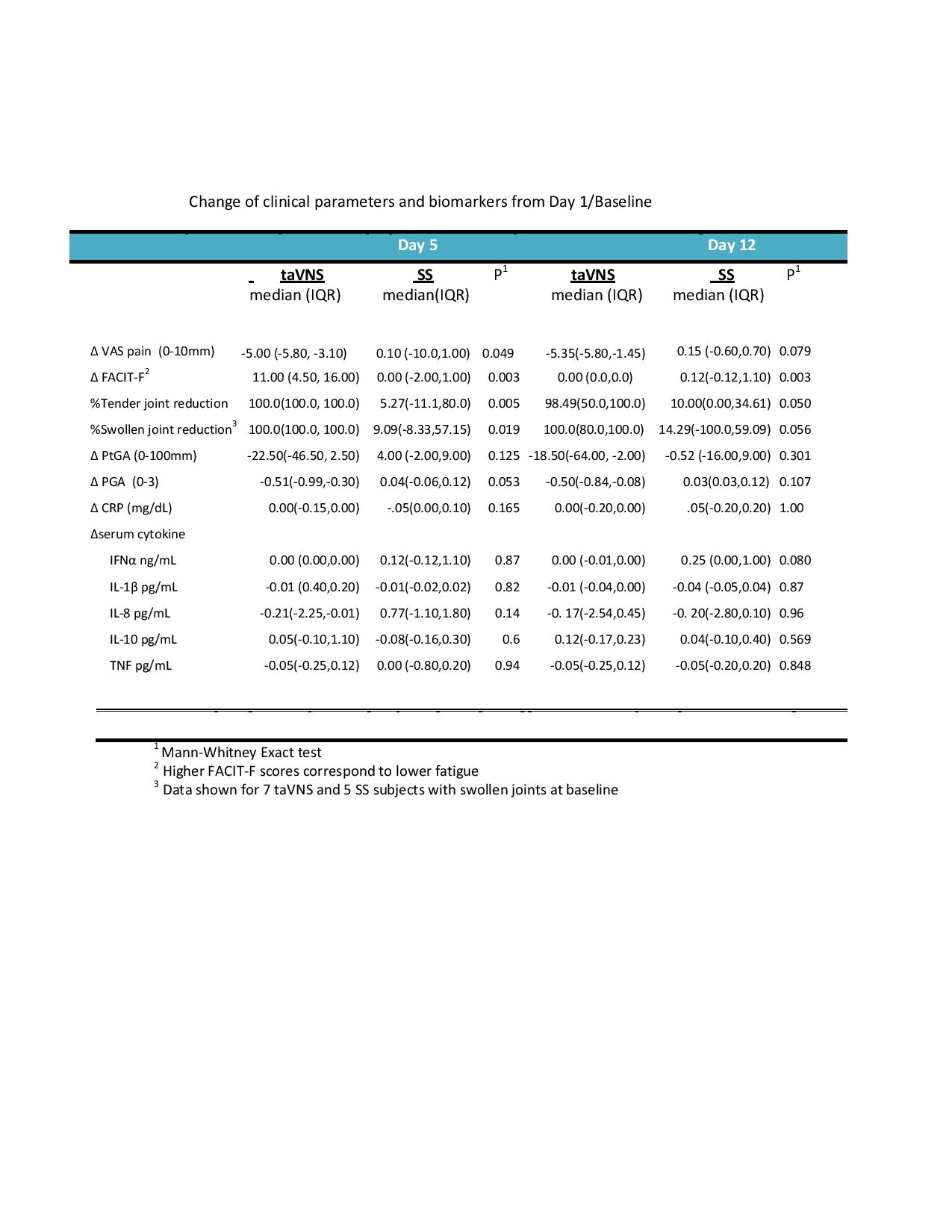
taVNS and SS were well tolerated with no significant adverse events in 19 enrolled subjects. Per protocol, 1 subject who withdrew after day 3 with a flu-like winter illness was replaced. Baseline characteristics of subjects receiving VNS or SS were similar. Following 4 consecutive days of stimulation, at day 5, subjects receiving VNS had a significant decrease in pain and fatigue compared to SS (Table 1), were more likely (OR =25 p=.02) to experience a minimal clinical significant reduction (1.58) in pain and were more likely to report improvement on a Likert scale. PtGA, joint counts and PGA were improved at day 5 in taVNS compared to SS subjects.. Pain reduction and improvement of fatigue correlated (R=0.49 p=.04, R=.83 p=.003 respectfully) with the average stimulation level. In general, response was maintained through day 12. Examination of serum and WBS biomarkers showed no significant differences at days 5 or 12 compared to baseline.
Conclusion:
To cite this abstract in AMA style:
Aranow C, Lesser M, Mackay M, Anderson E, Zanos TP, Datta-Chaudhuri T, Bouton C, Tracey KJ, Diamond B. Engaging the Cholinergic Anti-Inflammatory Pathway By Stimulating the Vagus Nerve Reduces Pain and Fatigue in Patients with SLE [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/engaging-the-cholinergic-anti-inflammatory-pathway-by-stimulating-the-vagus-nerve-reduces-pain-and-fatigue-in-patients-with-sle/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/engaging-the-cholinergic-anti-inflammatory-pathway-by-stimulating-the-vagus-nerve-reduces-pain-and-fatigue-in-patients-with-sle/