Session Information
Date: Tuesday, November 12, 2019
Title: RA – Diagnosis, Manifestations, & Outcomes Poster III: Comorbidities
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: In RA patients, anxiety and depression are associated with higher disease activity and worse outcomes. We hypothesized that in RA patients, poorer mental health would also be associated with more frequent office communication.
Methods: Charts of RA patients who received care at a university arthritis center for at least 1 year between April and September 2018 were identified from 530 records consecutively ordered by MRN (any arthritis type). Patients completed Patient Reported Outcome Measurement Information System (PROMIS) 29-item profiles (depression, anxiety, fatigue, physical function, pain interference, sleep disturbance, participation in social roles and activities) at an index care visit and phone calls and patient portal messages to rheumatologists and other providers were summed from the preceding 12 months. Patients were stratified by telephone call volume (none vs >=1). Demographics, clinical characteristics, and frequency of communication were compared between groups using t-tests or chi-square; Poisson regression was used to evaluate the relationship between emotional distress and telephone frequency, controlling for age, sex, race, RA disease duration, clinical disease activity index (CDAI), and PROMIS physical function, social participation, sleep disturbance, pain interference, and fatigue. A sensitivity analysis was performed controlling for use of anti-depressants (AD) and benzodiazepines (BZD).
Results: 154 out of 185 RA patients met 2010 ACR criteria, completed PROMIS profiles, and had a complete CDAI; 1,452 office communications were accrued. Patients were mostly female (n=110, 71%) and white (n=109, 71%) with a mean age (SD) of 59 (14). The median RA disease duration (IQR) was 8 years (5, 16), and median CDAI (IQR) was low at 7.5 (4, 19). High anxiety was present in 24% of RA patients, and high depression symptoms in 18%. RA patients with >=1 versus no telephone calls were mostly female, tended to be older, have more disease activity, and take ADs (Table 1). In multivariable Poisson regression, age (IRR=1.04, p< 0.01), race (IRR=1.75, p=< 0.01), social participation (IRR=0.95, p< 0.01), sleep disturbance (IRR=1.02, p=0.01), and anxiety (IRR=1.03, p< 0.01) were significantly associated with telephone call volume (any provider) (Table 2). Depression was associated with call volume in univariate analysis (IRR=1.04, p< 0.01) with a trend in multivariable analysis (IRR=0.98, p=0.06). In sensitivity analysis when controlling for use of AD and BZD, anxiety and depression continued to significantly impact call volume.
Conclusion: Office communication is driven by emotional and social determinants of health and not RA disease activity, duration, or disability. Patients with high anxiety or depression symptoms telephoned significantly more often than those with low symptoms, although this was not necessarily directed towards the rheumatologist. Early identification of anxiety and depression symptoms may prompt implementation of multi-modal strategies to address these symptoms and to provide additional information to alleviate patient concerns regarding their health.

ACR Office Communication Abstract_Table 1
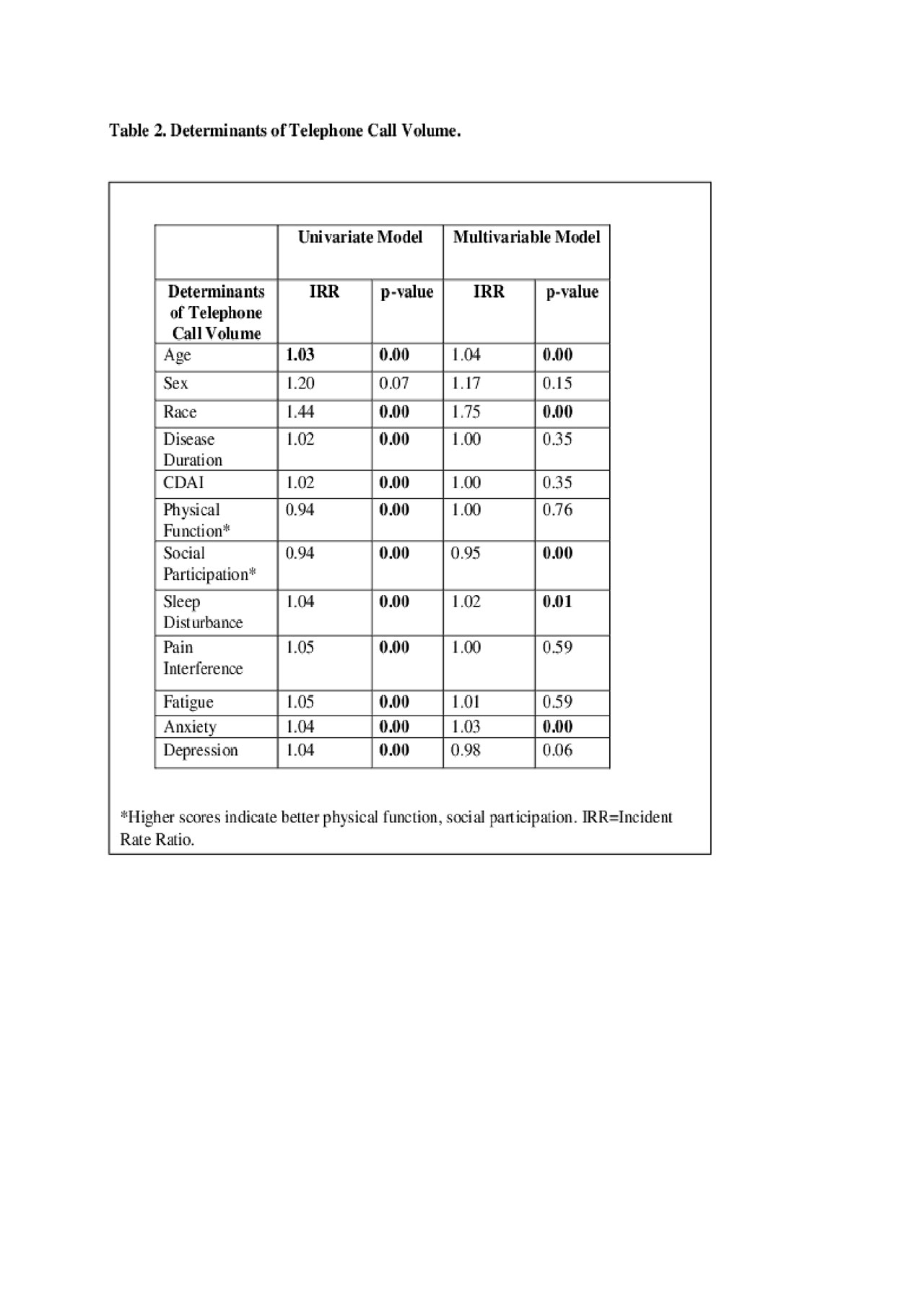
ACR Office Communication Abstract_Table 2
To cite this abstract in AMA style:
DiRenzo D, Wu M, Grader-Beck T, Bartlett S, Bingham C. Emotional and Social Determinants of Health Increase Office Communication for Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/emotional-and-social-determinants-of-health-increase-office-communication-for-patients-with-rheumatoid-arthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/emotional-and-social-determinants-of-health-increase-office-communication-for-patients-with-rheumatoid-arthritis/
