Session Information
Session Type: Abstract Session
Session Time: 2:00PM-3:30PM
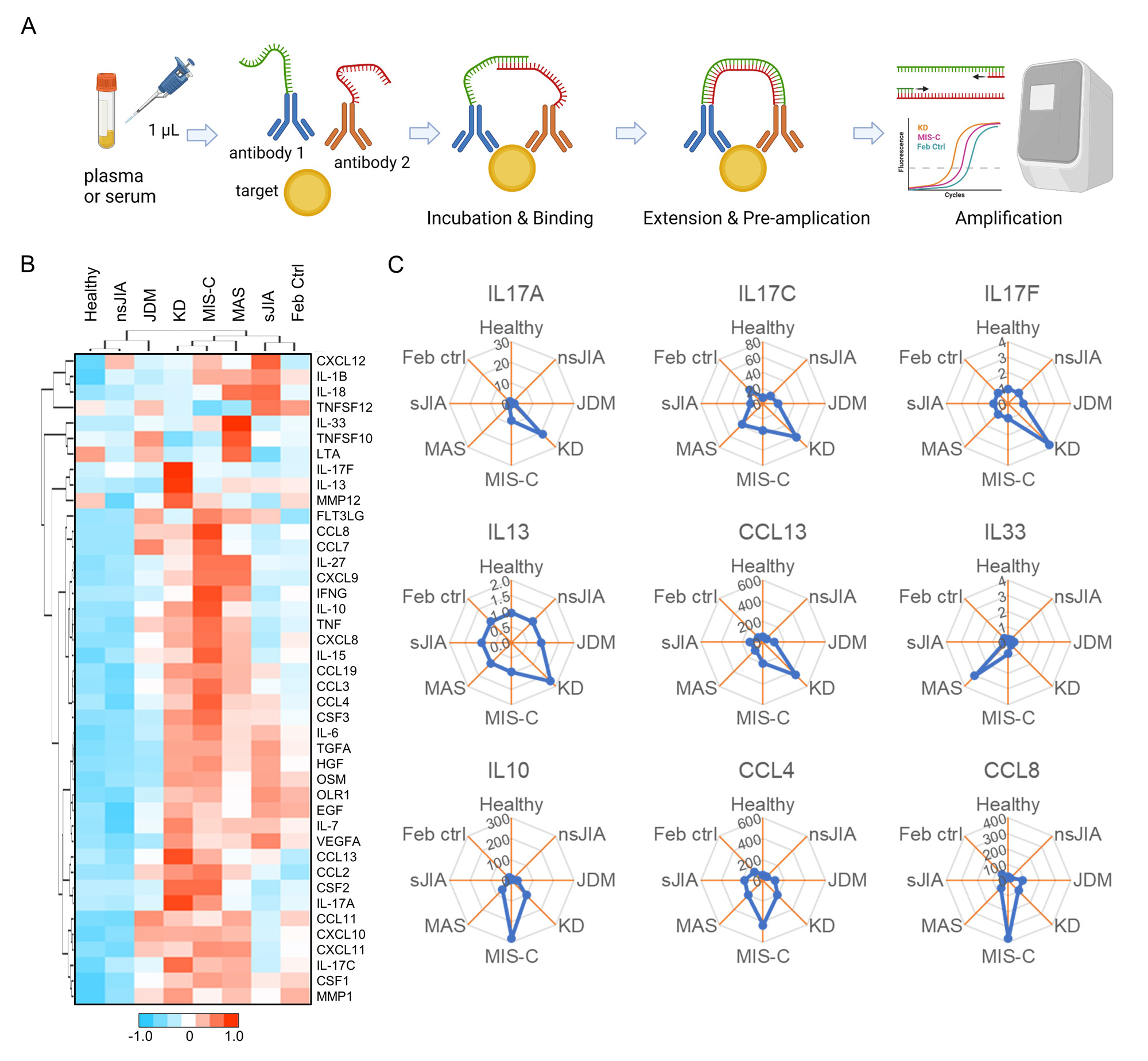
Background/Purpose: Kawasaki disease (KD) is a systemic vasculitis of young children that can lead to the development of coronary artery aneurysms (CAA) in up to 20% of patients. As KD shares overlapping clinical features with other pediatric inflammatory conditions, we aimed to identify diagnostic markers to distinguish KD using the proximity extension assay (PEA) proteomics platform that accurately quantifies protein targets in small volumes of biological fluids (Figure 1A).
Methods: We used PEA to profile proinflammatory mediators in plasma samples from healthy pediatric controls (n=30), febrile controls (n=26), and patients with KD (n=23), multisystem inflammatory syndrome in children (MIS-C; n=25), macrophage activation syndrome (MAS; n=13), systemic- and non-systemic juvenile idiopathic arthritis (n=14 and n=10, respectively), and juvenile dermatomyositis (n=9). We validated the key findings using serum samples from additional patients with KD (n=37) and febrile controls (n=28).
Results: High-fidelity proteomic profiling by PEA revealed distinct patterns of cytokine and chemokine expression across pediatric inflammatory diseases (Figure 1B). Although KD and MIS-C exhibited many similarities, KD differed from MIS-C and other febrile diseases in that most patients exhibited elevation in one or more members of the IL-17 cytokine family, IL-17A, IL-17C, and IL-17F (Figure 1C). In contrast, the MIS-C group showed elevated levels of IL-10, CCL4 and CCL8, while IL-33 elevation was specifically observed in the MAS group.
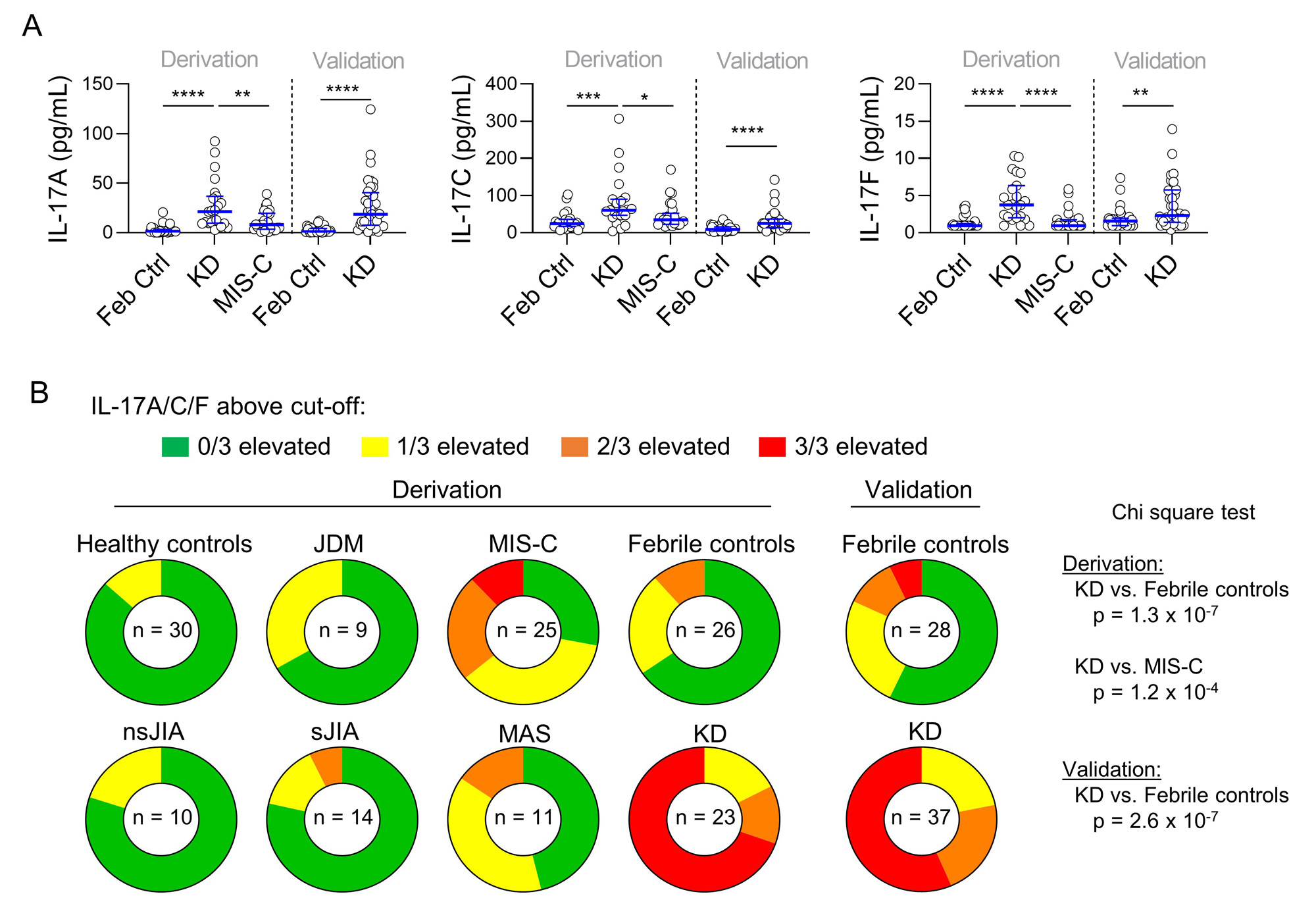
IL-17A, IL-17C, and IL-17F levels were significantly higher in patients with KD compared to those with MIS-C and febrile controls (Figure 2A). IL-17A was particularly sensitive and specific in discriminating KD from febrile controls with an area under the receiver operator characteristics (ROC) curve of 0.95 (95% CI: 0.89–1.00) in the derivation set and 0.91 (0.85–0.98) in the validation set. Concurrent elevation of all three IL-17-family cytokines was observed in >50% of KD patients (Figure 2B), including 19 of 20 with CAA, but was rare in other comparator groups. IL-17A and IL-17F levels were significantly higher in KD patients with CAA compared to those without CAA, whereas the levels of IL-1β, IL-6, and TNF were comparable between the groups.
Conclusion: Data from a single center demonstrated that elevation of IL-17-family cytokines is a hallmark of KD and may help to distinguish this pediatric vasculitis from its clinical mimics. Future multicenter studies are needed to validate these findings.
To cite this abstract in AMA style:
Brodeur K, Liu M, Du Y, Henderson L, Chang J, Newburger J, Nigrovic P, Lee P. Elevation of the IL-17 Cytokine Family Distinguishes Kawasaki Disease from Other Pediatric Inflammatory Disorders [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/elevation-of-the-il-17-cytokine-family-distinguishes-kawasaki-disease-from-other-pediatric-inflammatory-disorders/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/elevation-of-the-il-17-cytokine-family-distinguishes-kawasaki-disease-from-other-pediatric-inflammatory-disorders/