Session Information
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Depression has long been viewed as a comorbid condition in rheumatic diseases. Population studies have confirmed an increased incidence in patients with rheumatoid arthritis, systemic lupus erythematosus and systemic sclerosis. Additionally, studies have shown worse disease outcomes including increased mortality in patients with rheumatoid arthritis underscoring the need to identify and address depression in these populations.
This study assesses rates of screening and identifying depression after implementation of universal PHQ9 depression screening in an outpatient rheumatology clinic. We further evaluate any impact of rheumatologic diagnosis on rates of screening and explore provider beliefs on the role of the rheumatologist in addressing comorbid depression.
Methods: Universal PHQ9 screening was implemented in an outpatient rheumatology clinic consisting of physicians, physician assistants, and rheumatology fellows. Medical assistants would perform PHQ2 screens on all patients prior to their encounters and if positive would then perform full PHQ9 screens. If these were positive then the provider responsible for the encounter was notified and further triaging was left to their discretion.
A retrospective chart review of 16 random clinic dates between January 2020 and March 2020 was conducted. Race, age, gender and reason for clinic visit were collected. Each patient’s PHQ9 score was identified as well as their “established rheumatic disease” defined as what was entered into their reason for follow up by the provider or documented as such in the note. The chart was then reviewed to see if the provider responded to the screen by referring to a behavioral health liaison, adding this to the problem list, or discussing it in their assessment and plan. If none of these actions were done then the screen was considered to be “Not Addressed”.
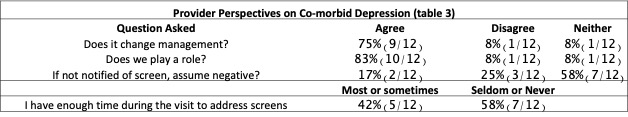
Also, an anonymous survey was performed to assess rheumatology provider beliefs pertaining to co-morbid depression screening.
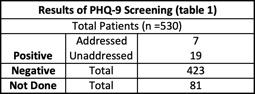
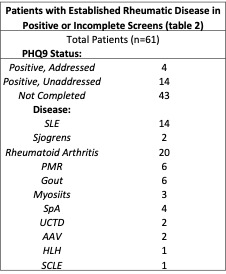
Results: Out of 530 patient visits, 432 had PHQ9 completed. 26/432 PHQ9 screens were positive (6%). Among positive screens, only 27% (7/26) were addressed (table 1). Out of the 18 patients with rheumatic disease that screened positive only 4 were addressed. There were also a large number of patients with rheumatic disease (43) who did not have screening performed at all despite clinic protocol (table 2). Out of the 12 providers that completed the survey the majority felt that co-morbid depression changed management (75%) and that they played a role (83%). 58% of providers felt they seldom or never had time to address the screens (table 3).
Conclusion: In spite of universal screening and the in office presence of a behavioral health liaison, the majority of positive PHQ9 results were not addressed. This trend remained true in patients with established rheumatic diseases suggesting that although providers recognize the importance of co-morbid depression there remains a care delivery gap in this subset of patients even with the addition of extra protocols and resources.
To cite this abstract in AMA style:
Bhatty O, Lucke M. Efficacy of Universal Depression Screening in a Rheumatology Clinic [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/efficacy-of-universal-depression-screening-in-a-rheumatology-clinic/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/efficacy-of-universal-depression-screening-in-a-rheumatology-clinic/