Session Information
Date: Sunday, October 26, 2025
Title: (0593–0640) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic lupus erythematosus (SLE) is associated with up to a three-fold increased risk of myocardial infarction (MI) and stroke. Statins have well-established cardioprotective benefits among non-SLE patients with atherosclerotic cardiovascular disease (ASCVD), but data assessing their efficacy for the secondary prevention of ASCVD in this population are scarce.
Methods: We specified and emulated a pragmatic target trial to compare outcomes among SLE patients initiating versus not initiating a statin following their first clinical ASCVD event. We identified an SLE cohort from TriNetX, a large electronic health record (EHR) database in the United States. We included patients with SLE (≥2 ICD codes ≥30 days and ≤2 years apart) between January 2002 and August 2021 who had a first clinical ASCVD event, including acute MI, coronary artery disease requiring intervention, unstable angina, ischemic stroke, or transient ischemic attack (TIA), identified by ICD codes during an inpatient or emergency room encounter. We excluded patients treated with a statin in the year preceding the index ASCVD event or with a contraindication. We compared the treatment strategies of statin initiation within 30 days after the index event versus no statin initiation. Study follow up commenced at the date of statin initiation or a randomly assigned date within the same 30-day period for non-initiators. We employed propensity score overlap weighting to emulate randomization. Covariates included demographics, type of index ASCVD event, comorbidities, SLE disease manifestations, medications, and healthcare utilization. Efficacy outcomes included all-cause death, major adverse cardiovascular events (MACE), and new-onset end-stage kidney disease (ESKD). We assessed the control outcome of injury/trauma. We utilized Cox regression to compare incidence rates between the two groups and employed a primary per-protocol approach, censoring patients upon deviation from their assigned treatment, and an intention-to-treat (ITT) approach as a secondary analysis.
Results: There were 1736 patients with SLE who met the inclusion/exclusion criteria (Figure 1). Of these, 726 patients initiated a statin, compared with 1010 non-initiators (Table 1). Baseline covariates were similar across both groups following propensity sore overlap weighting (standard difference < 0.001). The mean age was 53 years; 85% were female. In the per-protocol and ITT analyses, statin users had a lower risk of all-cause death (HR 0.55 [95% CI 0.34-0.91] and 0.53 [95% CI 0.34-0.82], respectively, Table 2). There was no difference in the risks of MACE (HR 0.96 [0.77-1.21], ESKD (HR 1.26 [95% CI 0.77-2.08]), or the control outcome of injury/trauma (HR 0.97 [95% CI 0.71-1.33]).
Conclusion: In this emulated target trial using a large, EHR-based cohort of patients with SLE and clinical ASCVD, we identified a lower risk of all-cause death associated with initiating a statin, although there were no significant differences in rates of MACE or ESKD. This study is limited by the possibility of residual bias and the use of administrative codes. These findings underscore the role for statin treatment in patients with SLE and ASCVD.
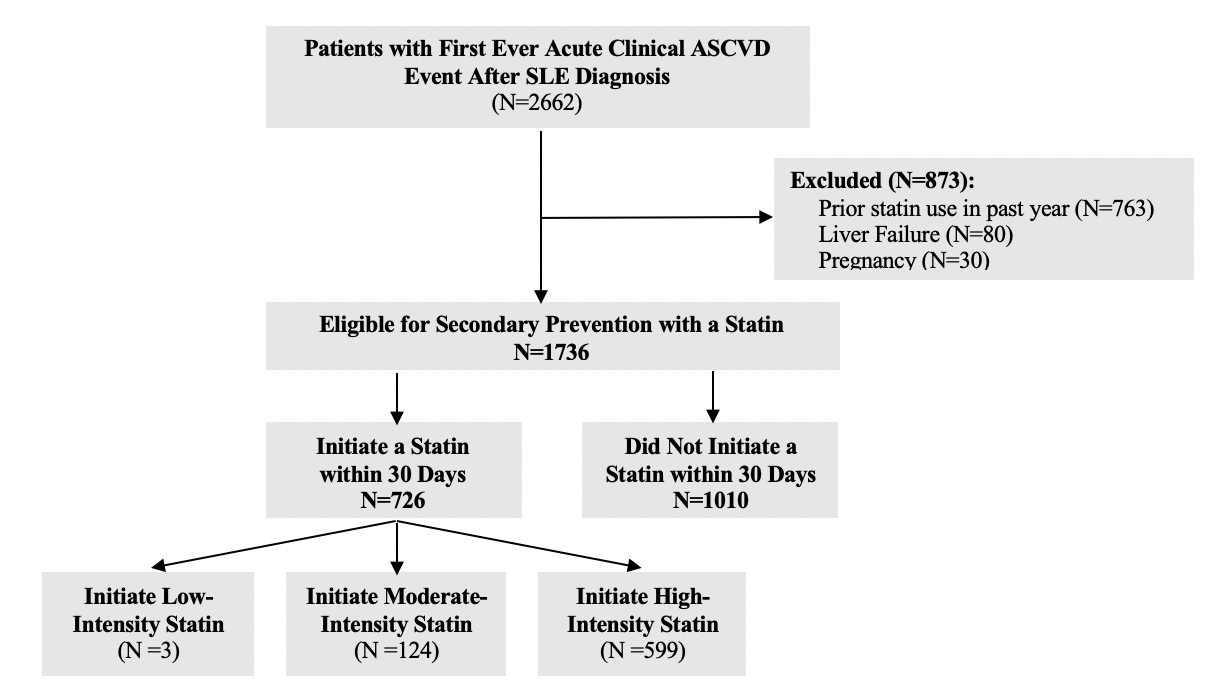 Figure 1. Consort Diagram of Entry into the Study
Figure 1. Consort Diagram of Entry into the Study
.jpg) Table 1. Baseline Characteristics of Statin Initiators and Non-Initiators with Systemic Lupus Erythematosus Following an Atherosclerotic Cardiovascular Disease Event
Table 1. Baseline Characteristics of Statin Initiators and Non-Initiators with Systemic Lupus Erythematosus Following an Atherosclerotic Cardiovascular Disease Event
.jpg) Table 2. Outcomes Associated with Statin Initiation vs Non-Initiation Following an Atherosclerotic Cardiovascular Disease Event in Patients with Systemic Lupus Erythematosus
Table 2. Outcomes Associated with Statin Initiation vs Non-Initiation Following an Atherosclerotic Cardiovascular Disease Event in Patients with Systemic Lupus Erythematosus
To cite this abstract in AMA style:
Patel A, Zhang L, Lau E, Zhou B, Zhang Y, Choi H, Jorge A. Efficacy of Statin Medications for Secondary Prevention of Atherosclerotic Cardiovascular Disease Among Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/efficacy-of-statin-medications-for-secondary-prevention-of-atherosclerotic-cardiovascular-disease-among-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/efficacy-of-statin-medications-for-secondary-prevention-of-atherosclerotic-cardiovascular-disease-among-patients-with-systemic-lupus-erythematosus/
