Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
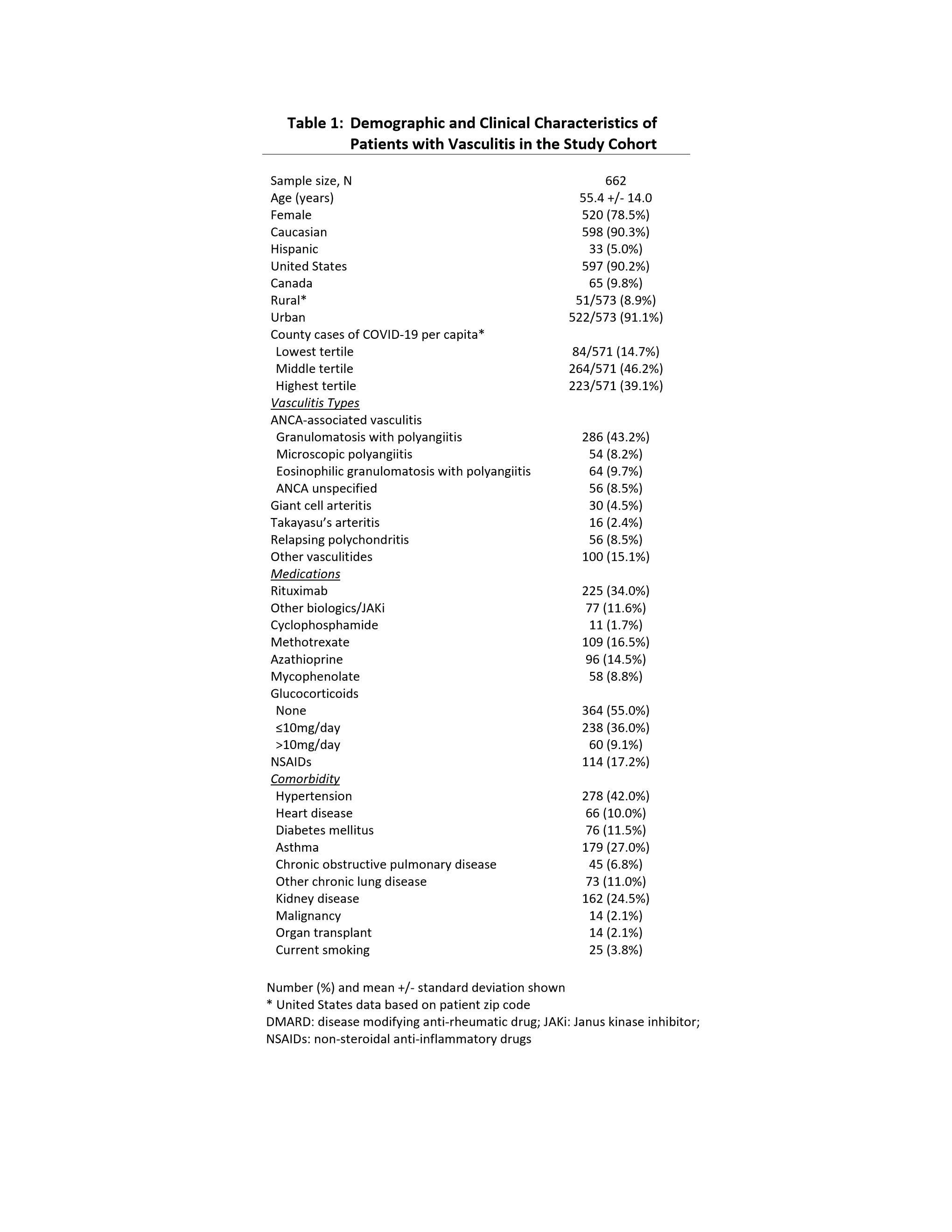
Background/Purpose: The COVID-19 pandemic has the potential to impact how patients with vasculitis interact with health care systems due to concerns about infections. This study aimed to analyze the concerns and health-related behaviors in patients with vasculitis during early phase of the COVID 19 pandemic in North America.
Methods: Patients with vasculitis were invited to complete an online survey through Vasculitis Patient-Powered Research Network in collaboration with the Vasculitis Foundation and the Relapsing Polychondritis Awareness and Support Foundation. Questions focused on concerns and behaviors related to doctors’ visits, laboratory and other tests, medication use, and telehealth use. Differences based on age, diagnoses, immunosuppressive drugs, daily glucocorticoid (GC) doses, urban vs. rural location, education, income, and COVID-19 infection rates in patients’ county were compared with Kruskal-Wallis (for concerns) or logistic regression, with telehealth analyses adjusted for date of survey completion. This report details findings from April 8, 2020 through May 29, 2020.
Results: Data from 662 patients were included: 90% Caucasians, 78% women (Table 1). Seven patients reported a diagnosis of COVID-19. Most patients (83%) expressed moderate or high levels of concern about COVID-19; 87% reported their vasculitis “moderately” or “extremely” affected their level of concern (Figure 1). Age >60 years (p< 0.01), female sex (p=0.01), and lung disease (p< 0.01) were associated with higher levels of concern. Immunosuppressive drug use and lung disease were associated with a higher likelihood that underlying vasculitis significantly affected level of concern (p< 0.01 each).
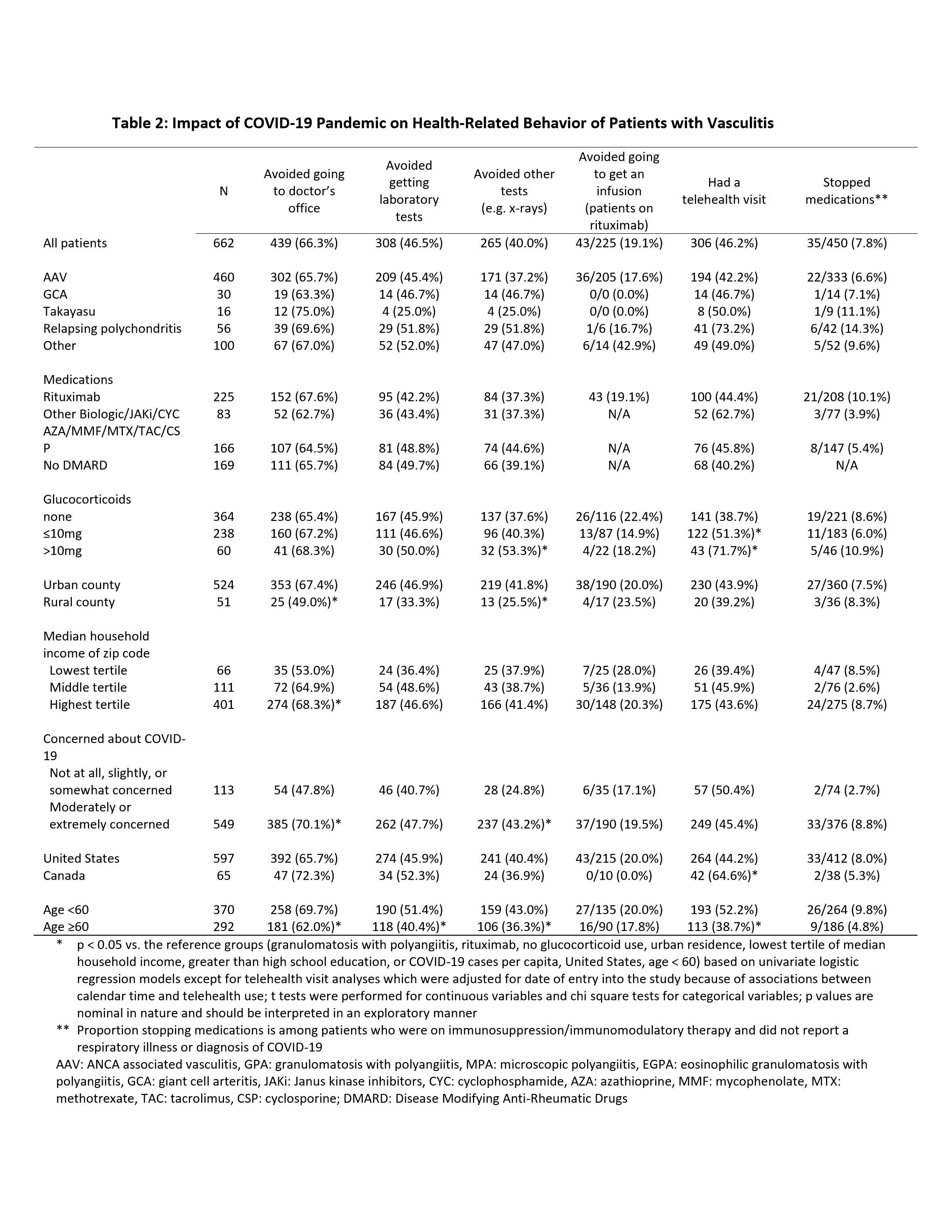
66% of patients reported avoiding doctors’ visits, 46% avoided laboratory tests, and 40% avoided other tests. Age < 60 years, urban location, higher COVID-19 activity, higher income, higher concern levels, and prednisone dose >10 mg/day were each associated with greater likelihood of avoiding visits or tests. 10% of patients on immunosuppression stopped drugs, especially patients with respiratory illnesses (39% vs 8% without respiratory illness, p< 0.01). The most common reasons for drug stoppage were concern about infection (57%) and physician’s advice (40%). Among 225 patients on rituximab, 43 (29%) reported avoiding an infusion.
44% of patients had telehealth visits; more visits were reported in younger patients, those on GC, and in Canada vs the USA (Table 2). Patients with telehealth visits were more likely to report getting information about COVID-19 from healthcare providers (65% vs 38%, p< 0.01).
Conclusion: In patients with vasculitis there were high levels of concern due to COVID-19 in the early months of the pandemic. Many patients avoided doctors’ visits, laboratory and other tests, and stopped or delayed medications without consulting physicians. Healthcare utilization varied across demographics and geographies. Strategies to facilitate ongoing engagement with the health care system during the pandemic are warranted and should be tailored to specific subsets of patients with vasculitis.
To cite this abstract in AMA style:
Banerjee S, George M, Young K, Venkatachalam S, Gordon J, Burroughs C, Curtis D, Ferrada M, Gavigan K, Grayson P, Kullman J, Curtis J, Shaw D, Nowell W, Merkel P. Effects of the COVID-19 Pandemic on Patients Living with Vasculitis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/effects-of-the-covid-19-pandemic-on-patients-living-with-vasculitis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/effects-of-the-covid-19-pandemic-on-patients-living-with-vasculitis/