Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
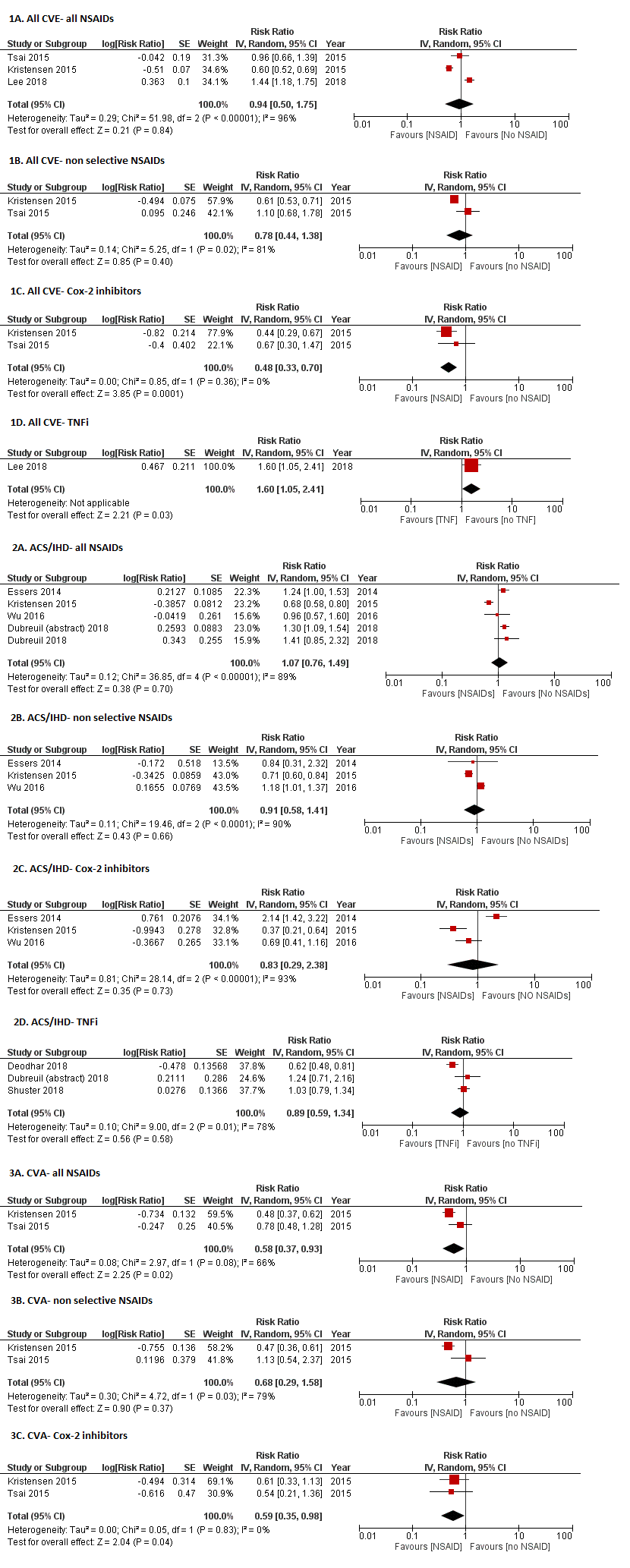
Background/Purpose: Most studies show a significantly higher risk of myocardial infarction [MI] (odds ratio [OR] = 1.60) and stroke (OR = 1.50) in ankylosing spondylitis (AS) patients. Whether therapies targeted at controlling inflammation may potentially reduce the risk of cardiovascular events (CVE) in AS, is not well understood. While NSAIDs are known to be associated with an increased risk of CVE in the general population, whether the anti-inflammatory effects of NSAIDs reduce or modify CVE risk in AS is controversial. It is also unclear if CVE risk is reduced by TNF inhibitors (TNFi), which has been shown in rheumatoid arthritis (RA). We aimed to perform a systematic review and meta-analysis to explore the association between NSAIDs, TNFi and CVE in AS.
Methods: We conducted a comprehensive search of several databases from inception to January 16, 2019. We included studies of patients with AS treated with NSAIDs, non-biological DMARDs or biologics, and had a control group. Outcomes of interest were all CVEs, myocardial infarction, stroke, congestive heart failure (CHF), and the composite outcome of major adverse cardiac events (MACE). Reported ORs and hazard ratios reported were converted to risk ratios (RR) using validated statistical formulae. Study specific RR were pooled using random-effects model (DerSimonian and Laird). Between-study heterogeneity was assessed using I2 statistics.
Results: Nine nonrandomized studies from a total of 1,425 studies screened fulfilled the inclusion criteria (Figure 1). In NSAID users as a whole, no increased risk of CVE was noted; however, the risk of cerebrovascular accident (CVA) was significantly lower (RR: 0.58, 95% CI 0.37 – 0.93, I2=66%). Cox-2 inhibitor use was associated with reduced risk of all CVE (RR: 0.48, 95%CI 0.33 – 0.70, I2= 0%) and CVA (RR: 0.58, 95% CI 0.37 – 0.93, I2= 66%). Non selective NSAIDs did not show a significant association with risk of any CVE. There was only 1 study reporting all CVE with TNFi, which showed a slightly higher risk (RR: 1.60, 95%CI 1.05 – 2.41). Meta-analysis of 3 studies of MI specifically did not show a significant association with TNFi (RR: 0.88, 95%CI 0.57 – 1.35, I2=76%). Only 1 study each reported risk of CHF and MACE, which were both low in all NSAID groups (Table 1). The certainty in evidence in all estimates was low due to the studies being nonrandomized.
Conclusion: This systematic review suggests that Cox-2 inhibitors in AS patients are associated with a lower risk of the composite CVE outcome and CVA, unlike their use in the general population. Similarly, NSAID users as a whole and users of non-selective NSAIDS did not have higher risk of any CVE. No significant association between TNFi and MI was observed. More studies are needed to study the association between TNFi use and CVE in general to evaluate a possible protective role in AS.
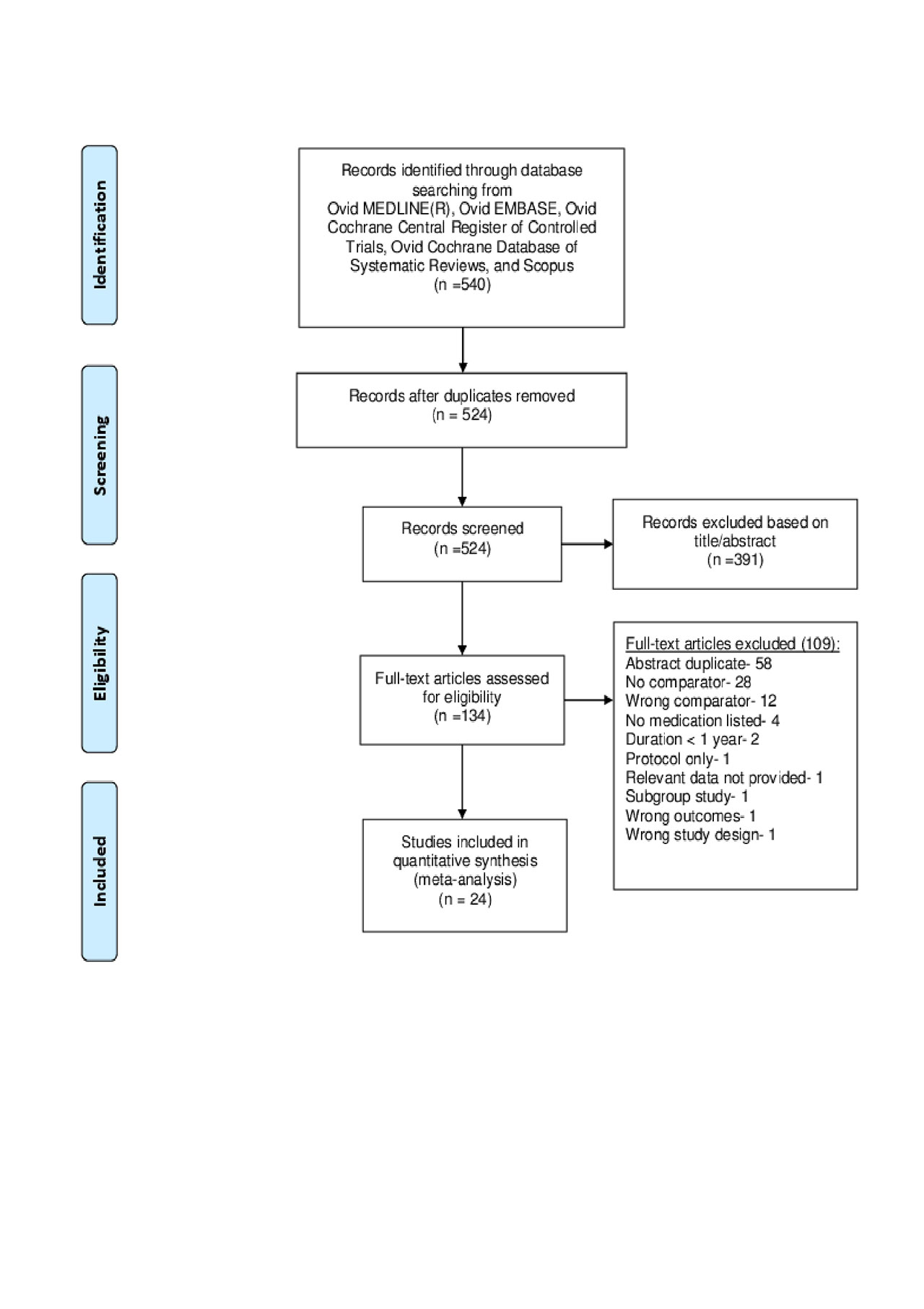
Figure 1-PRISMA diagram 5-30-19
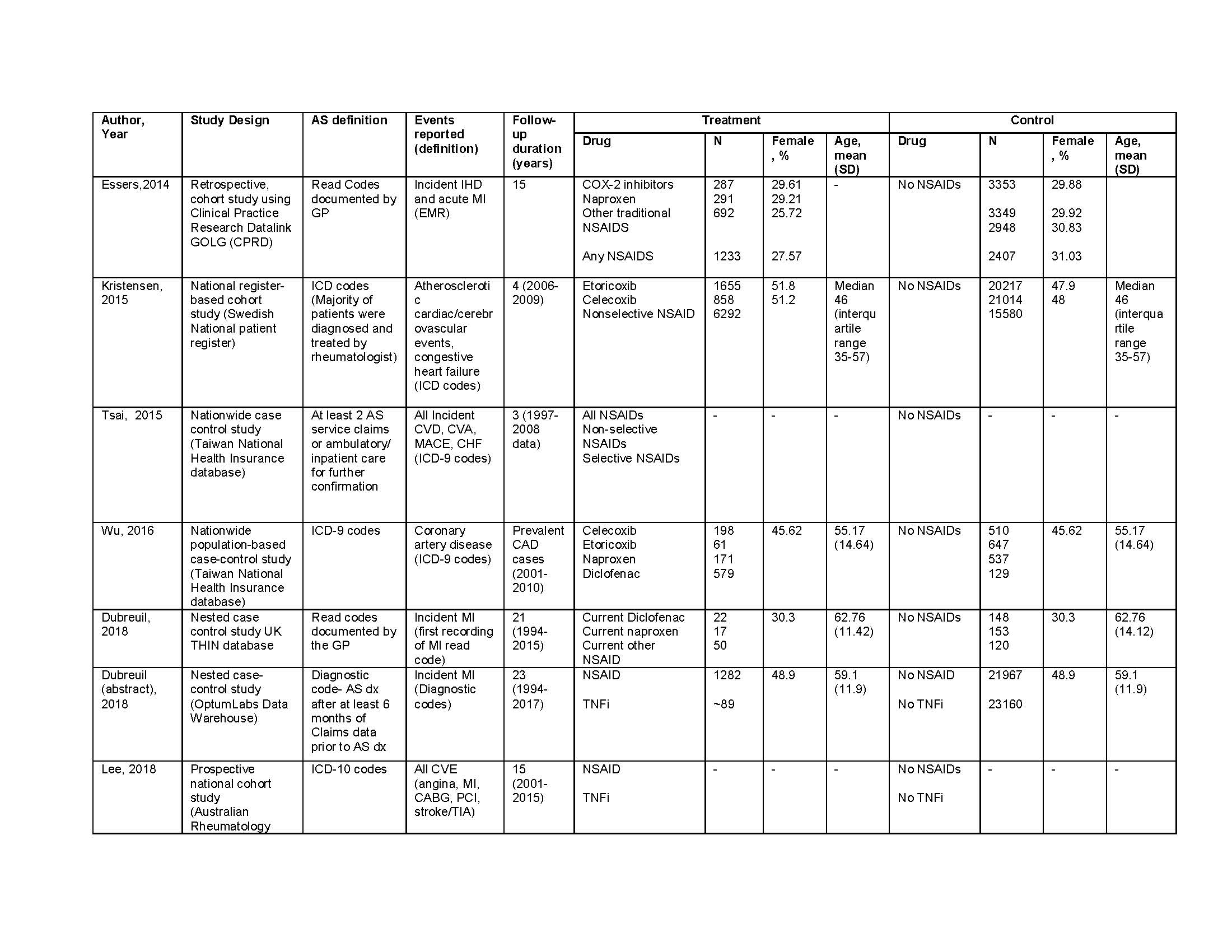
Table 1- baseline characteristics 6-01-19
To cite this abstract in AMA style:
Karmacharya P, Shahukhal R, Crowson C, Murad M, shrestha P, Bekele D, Wright K, Davis J, Dubreuil M. Effects of NSAIDs and TNF Inhibitors on Cardiovascular Events in Ankylosing Spondylitis: A Systematic Review and Meta-Analysis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/effects-of-nsaids-and-tnf-inhibitors-on-cardiovascular-events-in-ankylosing-spondylitis-a-systematic-review-and-meta-analysis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/effects-of-nsaids-and-tnf-inhibitors-on-cardiovascular-events-in-ankylosing-spondylitis-a-systematic-review-and-meta-analysis/