Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Obesity is associated with higher disease activity and poor treatment response in patients with psoriatic arthritis (PsA). However, there is limited data as to how weight loss strategies affect outcomes in PsA. The aim of our study was to compare joint surgery hospitalizations (as a surrogate marker of significant radiographic damage and progression) among (1) obese and non-obese PsA patients; (2) obese PsA patients without and with a history of bariatric procedure and subsequent weight loss.
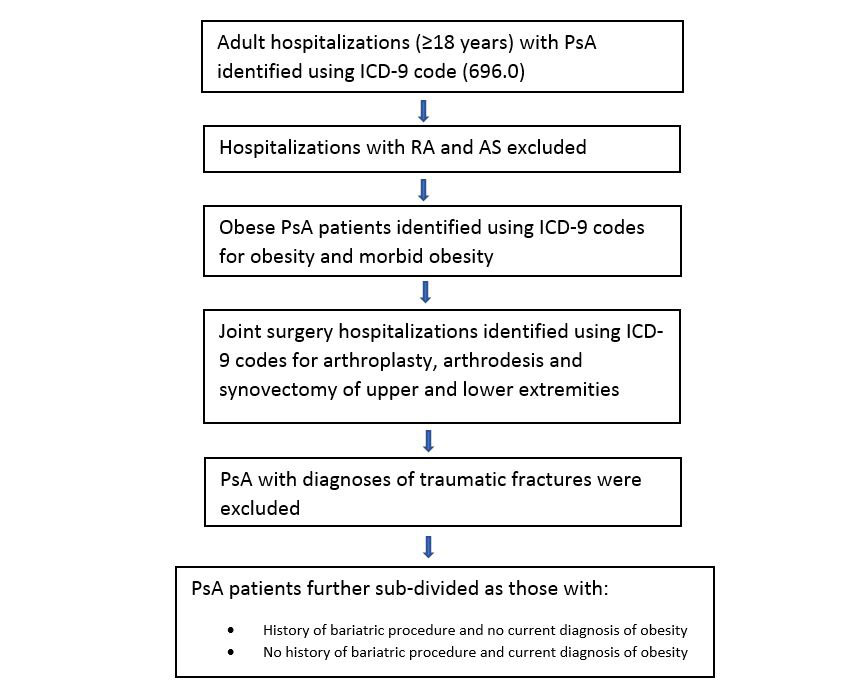
Methods: National Inpatient Sample (2001-2014) was used to identify patients ≥ 18 years with PsA using ICD-9 code 696.0. To increase the specificity, we excluded patients with RA (ICD-9 code 714.0) and AS (ICD-9 code 720.0) (Figure 1). For each patient with PsA, a matched control of the same age (± 1 year), sex, race/ethnicity and NIS stratum (based on hospital’s census region or division, ownership/control, location/teaching, and bed size) was randomly selected. We compared hospitalizations for joint surgeries among obese and non-obese PsA patients. Joint surgeries related to trauma/fracture were excluded. Secondly, we performed univariate and multivariate regression to compare joint surgery hospitalizations among PsA patients with a history of bariatric procedure vs. those without bariatric procedure. For this analysis, hospitalizations prior to 2006 were excluded as the ICD-9 code for history of bariatric procedure (V45.86) did not exist. Patients with current hospitalization for bariatric surgery were excluded to avoid confounding in the time gap between surgery and weight loss. Patients with a diagnosis of obesity were excluded from the group with a history of bariatric procedure in order to identify post-bypass patients who were no longer obese.
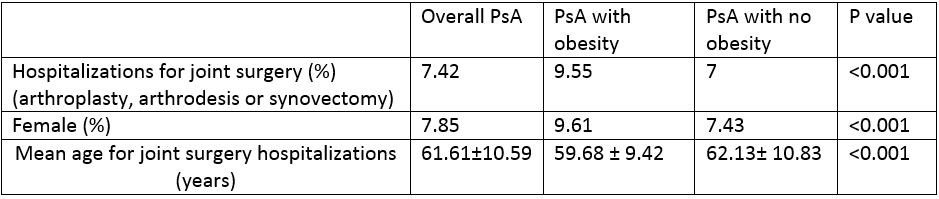
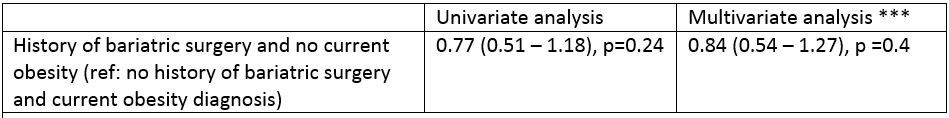
Results: In 2001-2014, there were 266,096 PsA hospitalizations. Among them, 44,055 (16.6 %) PsA patients had obesity or morbid obesity compared to 11.6% in the general population (p < 0.001). The overall hospitalization for joint surgeries in PsA was 7.42%. The rates of joint surgeries were significantly different among obese versus non-obese PsA hospitalizations (9.55 % vs 7.0%, p< 0.001) (Table 1). Mean age of joint surgery was 59.68 ± 9.42 years vs. 62.13± 10.83 years (p< 0.001) in obese PsA compared to non-obese PsA patients (Table 1). In the years 2006-2014, a total of 1,640 (0.91%) PsA hospitalizations had a history of bariatric surgery with no current diagnosis of obesity. There was no significant difference in overall joint surgery hospitalizations among these surgically treated formerly obese patients compared to currently obese PsA patients with no history of bariatric surgery (OR 0.83, 95% CI 0.54 – 1.27, p=0.4)(Table 2).
Conclusion: Our study showed obese PsA patients had higher hospitalizations for joint surgeries compared to non-obese patients. However, no difference was noted in joint surgery hospitalizations among PsA patients without and with a history of bariatric procedure and not currently obese. While few studies have shown improvement in disease activity after weight loss, the benefit of weight loss might be more in early PsA. Further longitudinal studies should explore the short and long-term effect of weight loss on PsA disease outcomes.
*** Multivariate analysis adjusted for age, gender, insurance status, hypertension, diabetes mellitus, dyslipidemia, current smoking status, hospitalization year and NIS stratum
To cite this abstract in AMA style:
Dhital R, Poudel D, Donato A, Oladunjoye O, Karmacharya P. Effect of Obesity and Surgical Weight Loss on Joint Surgery Hospitalizations in Psoriatic Arthritis: Data from National Inpatient Sample [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/effect-of-obesity-and-surgical-weight-loss-on-joint-surgery-hospitalizations-in-psoriatic-arthritis-data-from-national-inpatient-sample/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/effect-of-obesity-and-surgical-weight-loss-on-joint-surgery-hospitalizations-in-psoriatic-arthritis-data-from-national-inpatient-sample/