Session Information
Date: Saturday, November 7, 2020
Title: SLE – Treatment Poster I
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Hydroxychloroquine (HCQ) has demonstrated a wide array of beneficial effects in patients with systemic lupus erythematosus (SLE), with regard to disease activity, flare rates, organ damage, survival, thrombosis, lipid profile, diabetes mellitus and bone metabolism. Most of the existing data assesses HCQ use as a dichotomous variable at a single time point in a patient’s disease process. We looked at lifetime cumulative HCQ doses in a cohort of SLE patients to gain a more comprehensive view of the relationship between HCQ use and damage accrual. It is important to better characterize the benefits and risks of prolonged HCQ use given ongoing concerns about antimalarial-induced retinal toxicity, which is a common reason for HCQ discontinuation.
Methods: We studied a prospective cohort of 244 adult patients who met the 1997 American College of Rheumatology (ACR) classification criteria for SLE. Patients received care at a university medical center and were followed over at least 10 years. The cumulative HCQ dose from time of enrollment to last known follow-up was calculated for each patient via retrospective chart review. This value was then divided by the number of years since their SLE diagnosis to give a lifetime yearly average HCQ dose. Quinacrine use was accounted for by using a conversation of 300 mg HCQ for every 100 mg quinacrine. Disease damage was assessed using SLICC/ACR Damage Index (SDI) scores at baseline, 3 years, and 5 years after enrollment. We also recorded the incidence of cardiovascular events (CVE), defined as coronary artery disease, myocardial infarction, ischemic stroke, transient ischemic attack (TIA), or peripheral artery disease. Chi-squared test was used for dichotomous variables and Student’s t-test for continuous variables. Spearman’s test was used to examine correlations between two continuous variables.
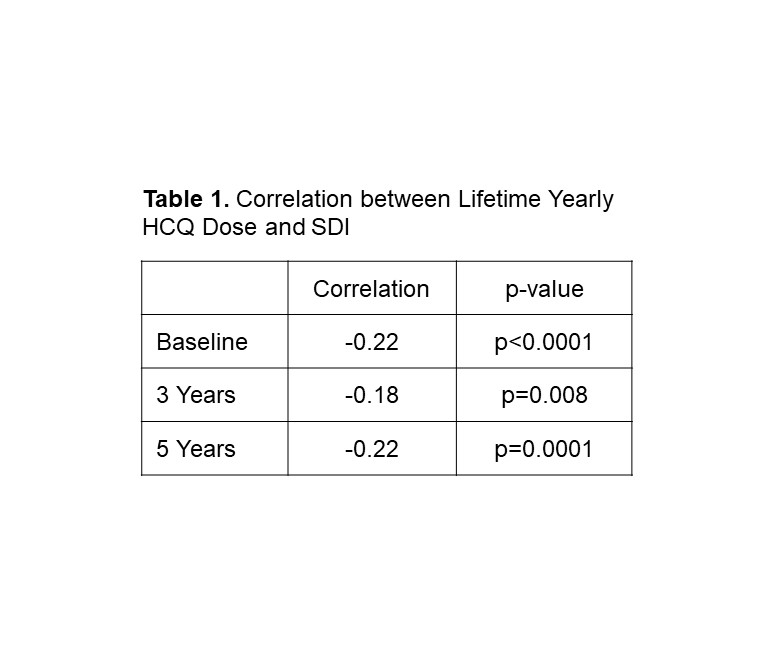
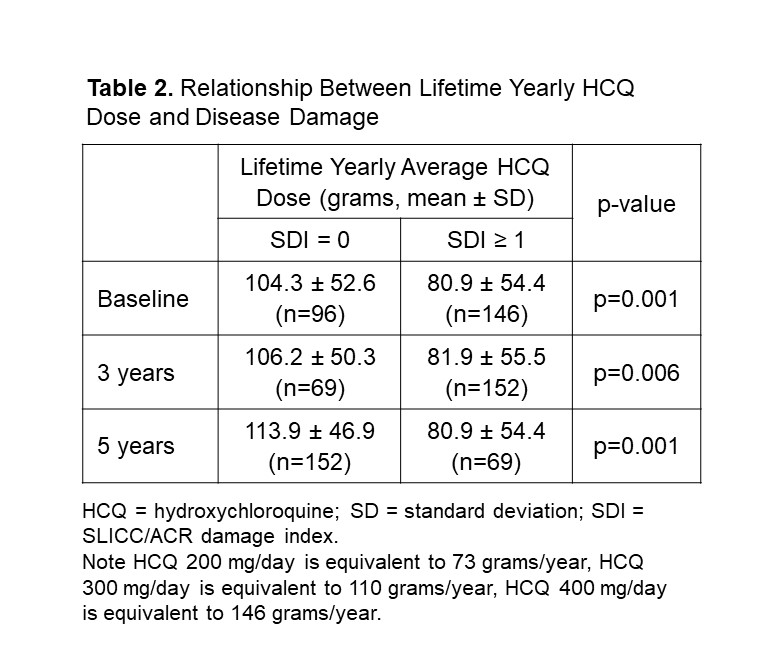
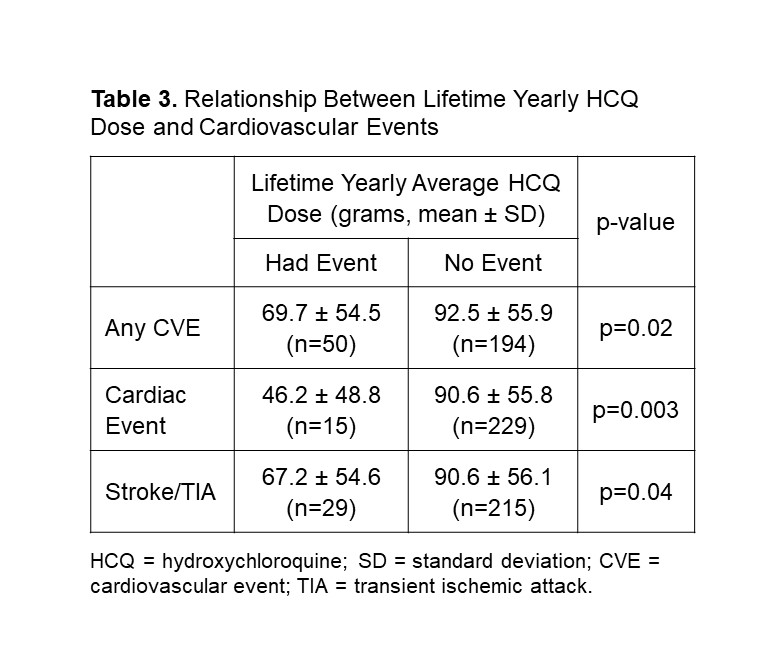
Results: The cohort was composed of 99% females, and the mean age of all patients was 40.7 years. There was a statistically significant negative correlation between lifetime yearly average HCQ dose and SDI at baseline, 3 years, and 5 years (Table 1). At all of these time points, patients who had an SDI of zero had a higher lifetime yearly average HCQ dose compared to patients who had an SDI of 1 or greater. These differences were all statistically significant (Table 2). Thirty-six of the 244 patients (18.8%) had at least one CVE during follow-up. Patients who did not have a CVE had a higher lifetime yearly average HCQ dose compared to patients who did have a CVE. The same pattern was seen when looking at cardiac events and ischemic stroke/TIA individually. These differences were all statistically significant (Table 3).
Conclusion: We found an inverse correlation between lifetime yearly HCQ dose and damage accrual in our cohort of patients with SLE. This was seen with regard to overall damage accrual as represented by the SDI, and specifically with cardiovascular damage as represented by CVE incidence. These findings reaffirm existing data on the benefits of HCQ use in SLE, and provide stronger support for the continuous use of HCQ at appropriate dosages over the course of disease unless clearly contraindicated.
To cite this abstract in AMA style:
Zhu L, Singh M, Siegel C, Sahakian L, Grossman J, McMahon M. Effect of Cumulative Hydroxychloroquine Dose on Prevention of Damage Progression in Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/effect-of-cumulative-hydroxychloroquine-dose-on-prevention-of-damage-progression-in-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/effect-of-cumulative-hydroxychloroquine-dose-on-prevention-of-damage-progression-in-patients-with-systemic-lupus-erythematosus/