Session Information
Date: Sunday, November 13, 2022
Title: SLE – Treatment Poster II
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Hydroxychloroquine (HCQ) has demonstrated benefit in multiple outcomes in systemic lupus erythematosus (SLE), including disease activity, flare rates, survival, and thrombotic events. Previous studies, however, assessed HCQ as a dichotomous variable and may have been confounded by discontinuation of HCQ in more severely ill patients. A better understanding of the impact of sustained HCQ use on key disease outcomes will allow clinicians to more accurately appraise the benefits and risks of continued use. We examined cumulative HCQ doses in a cohort of SLE patients to better assess the relationship with damage accrual. A lupus severity index (LSI) was employed to control for potential confounding from disease severity.
Methods: We studied a prospective cohort of 286 adult SLE patients, followed for a minimum of 10 years. The cumulative HCQ dose from time of diagnosis to last known follow-up was calculated via retrospective chart review. This value was then divided by SLE disease duration to give an average HCQ dose per year of disease duration (HCQ/yr). Disease damage was assessed using SLICC/ACR Damage Index (SDI) scores at baseline, 3, and 5 years after enrollment. The incidence of major adverse cardiovascular events (MACE) was defined as coronary artery disease, myocardial infarction, ischemic stroke, transient ischemic attack (TIA), or peripheral artery disease. A validated lupus severity index (LSI) was calculated. Student’s t-test and Spearman’s test were used for bivariate analysis. Logistic regression was used for multivariate analysis.
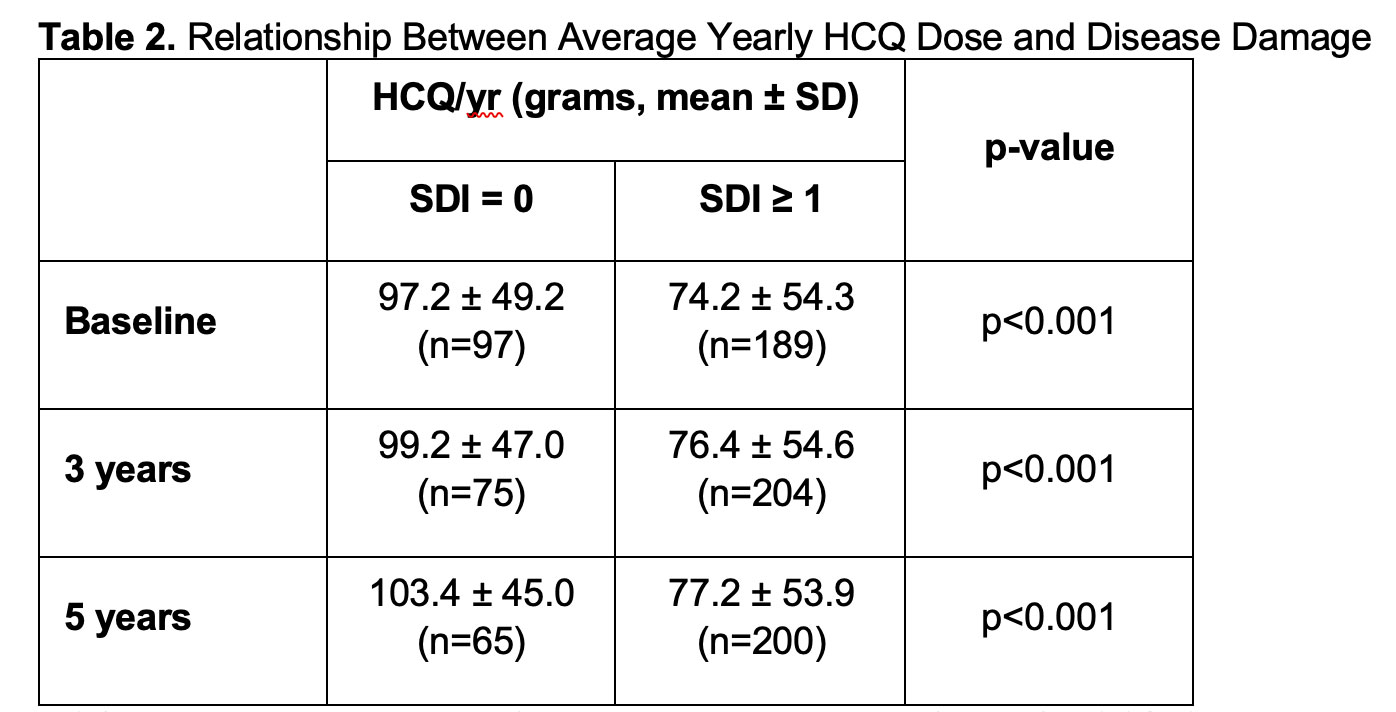
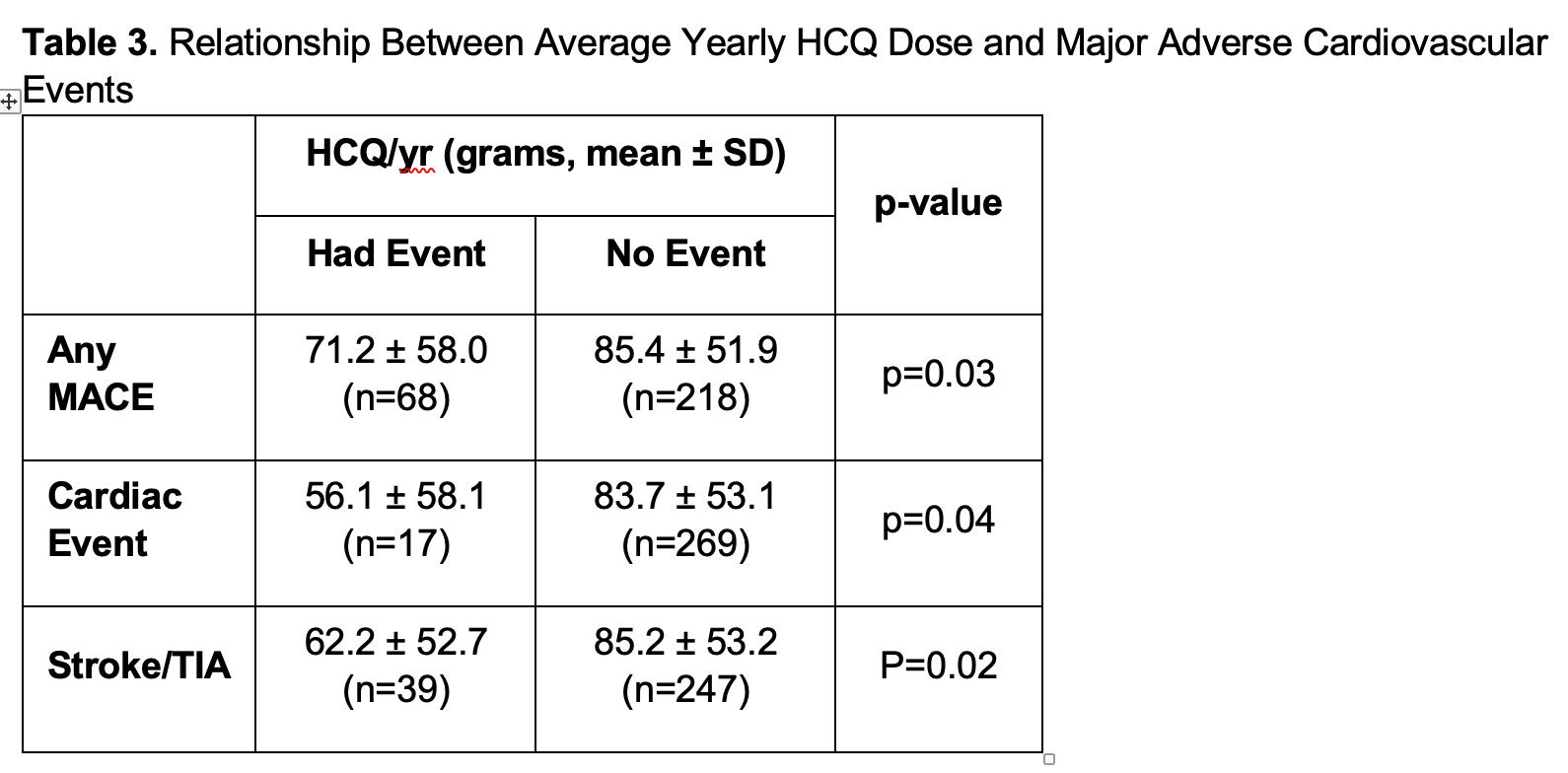
Results: The cohort was composed of 99% females (mean age 40.7 years). There was a statistically significant negative correlation between HCQ/yr and SDI at baseline, 3, and 5 years (Table 1). At all specified time points, patients with an SDI of zero had a higher mean HCQ/yr compared to patients with SDI >/=1 (p< 0.001)(Table 2). 68/286 (23.8%) of patients had at least one MACE during follow-up. Patients with a MACE had lower mean HCQ/yr compared to patients without MACE (p=0.03). The same pattern was seen when looking at cardiac events (p=0.04) and ischemic stroke (p=0.02)(Table 3). The LSI mean was significantly higher in patients with SDI >1 at baseline, 3, and 5 years (p < 0.009) and in patients with MACE (p=0.05). In a logistic regression model that included LSI and HCQ/yr, the odds of any MACE significantly decreased with higher mean HCQ/yr (OR 0.994, p=0.027).
Conclusion: We found an inverse association between average yearly HCQ dose and damage in our cohort of SLE patients. This was seen with overall damage accrual and more specifically with cardiovascular damage. When the LSI was applied to our cohort of patients, it proved to be a useful predictor of long-term damage accrual; however, when the LSI was applied as a potential confounder to the inverse association between higher mean HCQ/yr and MACE, the association was still significant. These findings reaffirm existing data on the benefits of HCQ use in SLE and provide additional support for the continuous use of HCQ at appropriate dosages over the course of disease unless clearly contraindicated.
Note: HCQ 200 mg/day is equivalent to 73 grams/year, HCQ 300 mg/day is equivalent to 110 grams/year, HCQ 400 mg/day is equivalent to 146 grams/year.
To cite this abstract in AMA style:
Jacquez J, Zhu L, Singh M, Siegel C, Sahakian L, Skaggs B, Grossman J, McMahon M. Effect of Cumulative Hydroxychloroquine Dose on Prevention of Damage Progression and Cardiovascular Events in Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/effect-of-cumulative-hydroxychloroquine-dose-on-prevention-of-damage-progression-and-cardiovascular-events-in-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/effect-of-cumulative-hydroxychloroquine-dose-on-prevention-of-damage-progression-and-cardiovascular-events-in-patients-with-systemic-lupus-erythematosus/