Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Macrophage activation syndrome (MAS) is a severe, life-threatening complication of rheumatologic disease. MAS is a form of secondary hemophagocytic lymphohistiocytosis which occurs most frequently in patients with Still’s disease (i.e., systemic juvenile idiopathic arthritis (sJIA) or adult-onset Still’s disease (AOSD)). MAS, if not properly treated, may progress to multiple organ failure and mortality. Treatment is aimed at achieving clinical stability and symptom resolution. However, there is currently no FDA approved therapy for MAS and corticosteroids remain the mainstay of treatment. Further, limited information exists regarding the economic burden (i.e., healthcare resource utilization (HCRU) and costs) of MAS in patients with Still’s disease in the United States.
Methods: A retrospective analysis of administrative claims (IQVIA PharMetrics Plus) from 2019 to 2024 was used to identify: Patients diagnosed with Still’s disease [(ICD-10:M082) including AOSD (ICD-10:M061) and sJIA (ICD-10:M08)] with ≥6 months of continuous enrolment prior to Still’s diagnosis (index date) and ≥12 months of continuous enrolment post-index without a MAS diagnosis (ICD-10:D76.1); and patients with Still’s disease with ≥6 months of continuous enrolment prior to earliest MAS diagnosis observed in the study period and ≥12 months of continuous enrolment post-MAS diagnosis. A propensity score was used to match patients (1:1) with Still’s disease with and without MAS. All-cause HCRU (inpatient [IP] admission, emergency room [ER] visits, and outpatient [OP] visits) and costs (all-cause and rheumatologic; adjusted to 2024 US dollars using the medical component of the Consumer Price Index) were ascertained in the post-index period. Differences in HCRU and costs were estimated using both unadjusted and adjusted analysis.
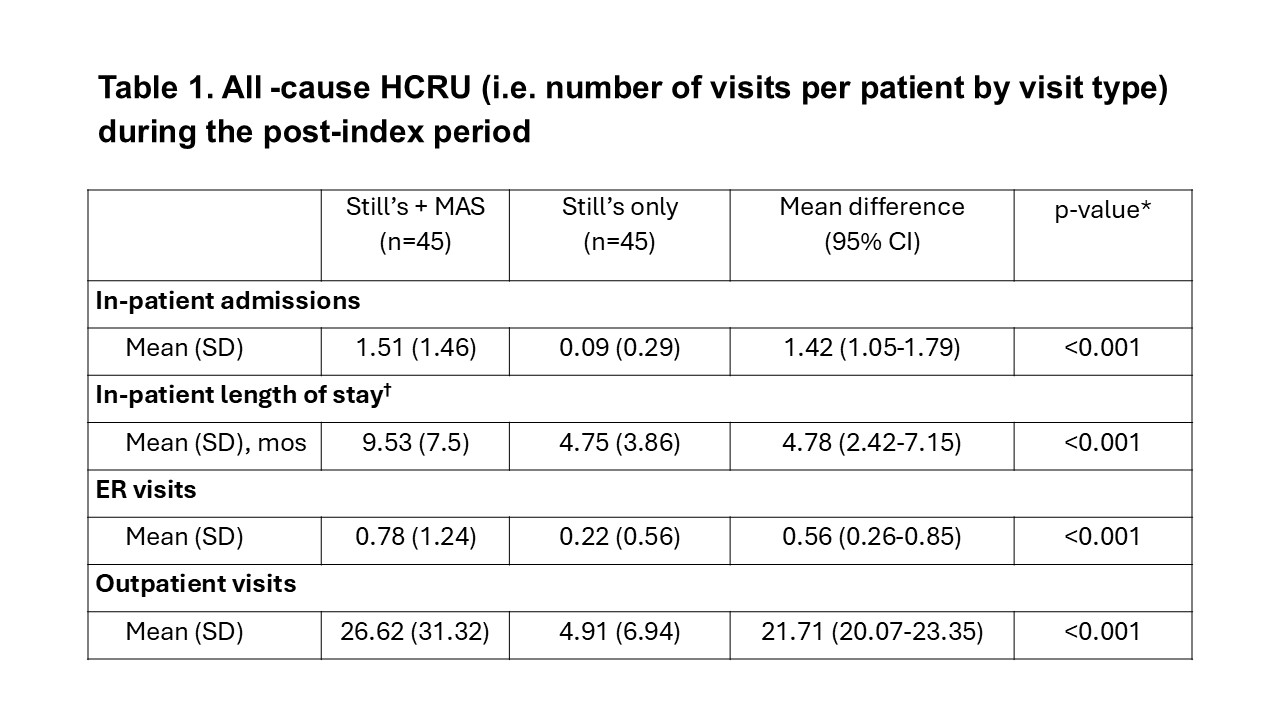
Results: After propensity score matching, 45 patients with Still’s and 45 patients with Still’s and MAS were included (mean [SD] age, 26.8 [15.1] and 26.8 [16.0] years at Still’s diagnosis, respectively; female, 55.6% and 60.0%, respectively). Mean (SD) Elixhauser Comorbidity Index was 1.6 (1.5) and 2.1 (2.8), respectively. The most common comorbidities were rheumatoid arthritis (48.9% and 42.2%) and cardiac arrythmia (13.3% and 22.2%) in patients with Still’s with and without MAS, respectively. Patients with MAS were significantly more likely to have an ER visit (P=0.04) and/or IP admission (P< 0.001) than patients without MAS in the 12-month post-index period (Figure 1). They also had significantly more frequent IP admissions (P< 0.001), ER visits (P< 0.001), OP visits (P=< 0.001), and longer IP stays (P< 0.001) than patients without MAS (Table 1). In addition, patients with MAS incurred significantly (P=0.008) higher total all-cause ($318,828 vs $19,233) and rheumatologic-related ($163,099 vs $1,930) healthcare costs (P=0.02) than patients without MAS (Table 2).
Conclusion: Patients with Still’s and MAS incurred significantly higher HCRU and associated costs compared with similar patients without MAS. Availability of novel therapies targeted to treat MAS may reduce the overall burden of disease to patients and the healthcare system.
 HCRU was measured during the observation period, defined as the 12-month post-index period. ORs were evaluated for binary variables (ie, at least one visit) using logistic regression. Models were controlled for age at Still’s diagnosis, underlying Still’s diagnosis (AOSD, sJIA), sex, and ECI during the baseline period. ORs >1 indicate higher odds for patients with Still’s and MAS compared with propensity score matched patients with Still’s without MAS.
HCRU was measured during the observation period, defined as the 12-month post-index period. ORs were evaluated for binary variables (ie, at least one visit) using logistic regression. Models were controlled for age at Still’s diagnosis, underlying Still’s diagnosis (AOSD, sJIA), sex, and ECI during the baseline period. ORs >1 indicate higher odds for patients with Still’s and MAS compared with propensity score matched patients with Still’s without MAS.
ECI= Elixhauser Comorbidity Index; CI=Confidence interval; ER= Emergency room; HCRU=Healthcare resource utilization; MAS=Macrophage Activation Syndrome; OR= Odds ratio.
.jpg) * Results remained robust when adjusted for age at Still’s diagnosis, underlying Still’s diagnosis (i.e., AOSD, sJIA), sex, and ECI
* Results remained robust when adjusted for age at Still’s diagnosis, underlying Still’s diagnosis (i.e., AOSD, sJIA), sex, and ECI
†Limited to patients with at least 1 in-patient admission
AOSD= Adult-onset Still’s disease (AOSD); CI= confidence interval; ECI= Elixhauser Comorbidity Index; ER=Emergency room; MAS= macrophage activation syndrome; MOS= Months; sJIA= Systemic juvenile idiopathic arthritis
.jpg) * Results remained robust when adjusted for age at Still’s diagnosis, underlying Still’s diagnosis (i.e., AOSD, sJIA), sex, and ECI
* Results remained robust when adjusted for age at Still’s diagnosis, underlying Still’s diagnosis (i.e., AOSD, sJIA), sex, and ECI
†Limited to patients with at least 1 in-patient admission
AOSD= Adult-onset Still’s disease (AOSD); CI=Confidence interval; ECI= Elixhauser Comorbidity Index; ER=Emergency room; MAS= macrophage activation syndrome; sJIA= Systemic juvenile idiopathic arthritis
To cite this abstract in AMA style:
Marrone M, McPherson C, Oladapo A. Economic Burden of Macrophage Activation Syndrome (MAS) in Patients with Still’s Disease (Systemic Juvenile Idiopathic Arthritis (sJIA) and Adult-onset Still’s Disease (AOSD)): Analysis of a US National Administrative Claims Database [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/economic-burden-of-macrophage-activation-syndrome-mas-in-patients-with-stills-disease-systemic-juvenile-idiopathic-arthritis-sjia-and-adult-onset-stills-disease-aosd-analysis-of-a/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/economic-burden-of-macrophage-activation-syndrome-mas-in-patients-with-stills-disease-systemic-juvenile-idiopathic-arthritis-sjia-and-adult-onset-stills-disease-aosd-analysis-of-a/
