Session Information
Date: Tuesday, November 9, 2021
Title: Systemic Sclerosis & Related Disorders – Clinical Poster III (1836–1861)
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Systemic sclerosis (SSc) is a complex disease characterized by microvascular abnormalities, immune dysregulation and chronic inflammation, and subsequent excessive fibrosis of the skin and internal organs. This leads to irreversible tissue remodeling and organ damage, resulting in increased morbidity and mortality. Recent accumulating evidence has shown that therapeutic disease modification is possible in SSc patients using immunomodulators. In rheumatoid arthritis, it has been shown that early disease is more susceptible to treatment, but we still don’t know whether therapeutic “window of opportunity” exists in SSc patients.
Methods: This was a single-center, retrospective study enrolling SSc patients who received disease-modifying therapy for diffuse cutaneous SSc (dcSSc) or interstitial lung disease (ILD). Eligible patients were selected from our SSc database, and included those who i) fulfilled the 2013 ACR/EULAR classification criteria for SSc; ii) received treatment with cyclophosphamide, mycophenolate mofetil or tocilizumab for dcSSc or ILD within 6 years after onset of non-Raynaud’s symptoms; and iii) had been on treatment for least one year. The patients were divided into early and late intervention groups based on the disease duration of ≤18 months or >18 months at treatment introduction. We evaluated changes of modified Rodnan total skin score (mRSS) and percent predicted forced vital capacity (ppFVC) from baseline to one year. Patients experiencing decrease of mRSS by ≥ 5 or relative increase of ppFVC by ≥10% were regarded as improvers. Clinical worsening was defined as development of at least one original or revised ACR-CRISS step 1 event or progressive fibrosing ILD (PF-ILD). Cumulative rates for clinical worsening were assessed using Kaplan-Meier analysis, and were compared between the groups with log-rank test.
Results: We enrolled 44 patients, including 24 in the early intervention group and 20 in the late intervention group. Disease duration at treatment introduction was 8.6 ± 4.2 and 34.3 ± 20.3 months in early and late intervention groups, respectively. Baseline characteristics were principally similar between the groups except ppFVC, which was significantly better in the early than late intervention group (93.2 ± 13.8 versus 80.4 ± 18.2; P < 0.05). There was no significant difference in changes of mRSS or ppFVC over one year between the two groups, but improvers tended to be more common in the early versus late intervention groups (37.5% versus 22.2% for mRSS, and 47.6% versus 16.7% for ppFVC). The Kaplan-Meier analysis revealed that the original and revised ACR-CRISS step 1 event tended to occur less frequently in the early than the late intervention group (P = 0.06 and P < 0.05, respectively; Figure 1). In addition, patients received early intervention developed PF-ILD less frequently, compared with those received late intervention (P < 0.05; Figure 2).
Conclusion: Our findings suggest that early intervention with immunomodulators in patients with dcSSc and/or SSc-ILD prevents clinical worsening, although further prospective study involving a larger number of patients is necessary to confirm the “window of opportunity” theory in the treatment of SSc.
 Figure1:Time to clinical worsening defined by original and revised ACR-CRISS step 1 event
Figure1:Time to clinical worsening defined by original and revised ACR-CRISS step 1 event
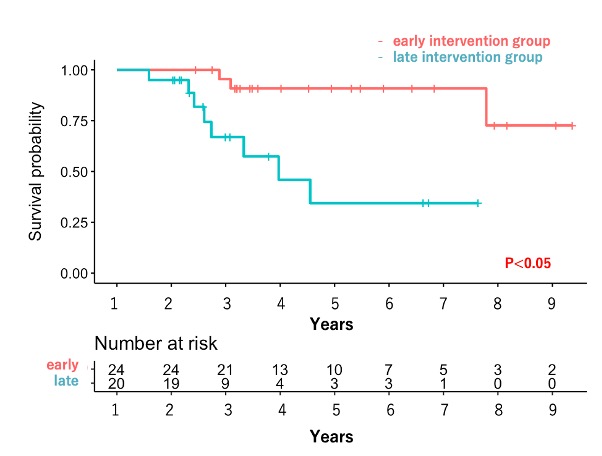 Figure2 : Time to clinical worsening defined by PF-ILD
Figure2 : Time to clinical worsening defined by PF-ILD
To cite this abstract in AMA style:
Yomono K, Kuwana M. Early Intervention with Immunomodulators Leads to Better Outcomes in Patients with Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/early-intervention-with-immunomodulators-leads-to-better-outcomes-in-patients-with-systemic-sclerosis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/early-intervention-with-immunomodulators-leads-to-better-outcomes-in-patients-with-systemic-sclerosis/
