Session Information
Date: Monday, November 8, 2021
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Giant cell arteritis (GCA) is the large and medium vasculitis that affects elderly people GCA frequently overlaps with polymyalgia rheumatica (PMR). PMR is a common rheumatic disease and it affects the proximal large joints in the shoulders and hips. Long-term glucocorticoids (GCs) administration is the main treatment option for GCA and PMR patients. However, GCs lead to GC-related adverse events including hypercholesterolemia, hypertension, diabetes mellitus, cataract, and infections. Therefore, new treatment options is required. Previous studies suggest a negative association between metabolic features cholesterol, blood glucose) and a BMI in the development of GCA. However, data are limited. In this study, we aimed to investigate the metabolic features, BMI in two independent GCA/PMR cohorts and elaborate the prevalence of comorbidities in GCA/PMR patients at the time of diagnosis and during treatment to stratify patients.
Methods: This study included two independent cohorts from Aarhus and Groningen (GPS cohort). The GPS cohort included 50 GCA and 44 PMR patients. As a background population, 50-93 years old participant of Lifelines cohort study was included. In addition, 52 GCA and 25 PMR patients from the Aarhus cohort were included. Baseline characteristics of GCA/PMR patients from the GPS cohort were compared with general population and patients in the Aarhus cohort. Patients in the GPS cohort were prospectively followed with visits at 3 months, 1, 2, 3, 4 and 5 years. Laboratory measurements, comorbidities (diabetes mellitus, hypercholesterolemia, hypertension, obesity and cataract) were assessed at every visit.
Results: In contrast to previous literature, higher HbA1c and glucose levels and lower LDL, HDL and cholesterol were detected in GCA patients than in general population. This suggested a dysregulation in lipid and glucose metabolism in GCA patients. Aarhus cohort was comparable with GPS cohort. Next, association of comorbidities with acute-phase markers at the time of diagnosis was investigated. GCA patients with cataract had reduced CRP and ESR whereas higher ESR was observed in PMR patients with cataract compared to patients without cataract. Analysis of GC treatment effect on comorbidities revealed a significant increase in diabetes and cataract in GCA patients, mainly after 3 months and 5 years, respectively, compared to baseline. BMI significantly increased 1, 4 years and 5 years after GC treatment initiation. Additionally, frequency of obese patients increased after 5years of GC usage in GCA patients.
Conclusion: Here we show that a disturbance in glucose and lipid metabolism in newly-diagnosed GCA patients. GC treatment resulted in the development of comorbidities and BMI in GCA patients, emphasizing the need for improved GC-sparing treatment options.
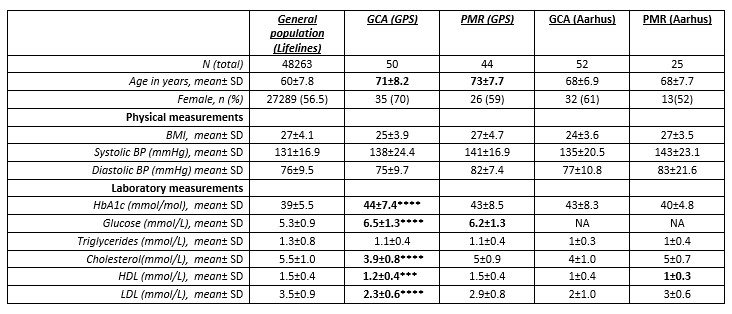 Table 1. Patient characteristics, laboratory tests, comorbidities and intoxications are shown. NA: not applicable.**** < 0.0001, *** < 0.001 corresponds to difference between GPS and Lifelines cohorts.
Table 1. Patient characteristics, laboratory tests, comorbidities and intoxications are shown. NA: not applicable.**** < 0.0001, *** < 0.001 corresponds to difference between GPS and Lifelines cohorts.
To cite this abstract in AMA style:
Esen I, Therkildsen P, Dalsgaard Nielsen B, van 't Ende A, Boots A, Heeringa P, Hauge E, Brouwer E, van Sleen Y. Dysregulated Glucose Metabolism and Dyslipidemia in GCA and PMR Patients at Diagnosis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/dysregulated-glucose-metabolism-and-dyslipidemia-in-gca-and-pmr-patients-at-diagnosis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/dysregulated-glucose-metabolism-and-dyslipidemia-in-gca-and-pmr-patients-at-diagnosis/
