Session Information
Date: Monday, November 18, 2024
Title: SpA Including PsA – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Psoriasis typically precedes psoriatic arthritis (PsA), with a variable transition period. In this study, we aimed to explore whether the time interval between the onset of psoriasis and PsA impacts the clinical phenotype at baseline and long-term outcomes.
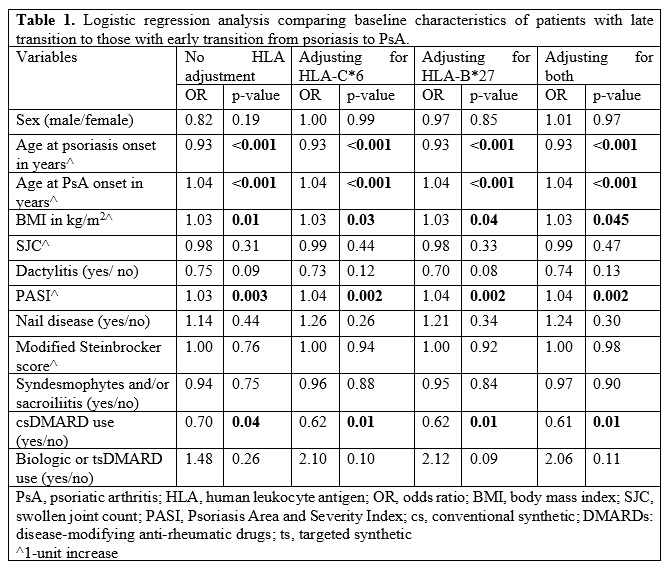
Methods: We included patients who developed PsA concurrently or after psoriasis and were enrolled in our prospective observational cohort within two years of the onset of PsA (inception cohort). We divided the cohort into early and late transition groups based on the median transition period of nine years. We used logistic regression analysis to compare baseline demographic and disease-related characteristics, with and without adjusting for human leukocyte antigen (HLA)-B*27 and HLA-C*06. We used multivariate linear regression for the 5-year adjusted mean swollen joint count (SJC) and Cox-proportional analysis for time to radiographic progression to explore the influence of early and late transition groups on disease activity and damage, respectively. We then performed the same analyses comparing patients with concurrent disease (PsA onset within one year of psoriasis) to the rest of the cohort (non-concurrent disease).
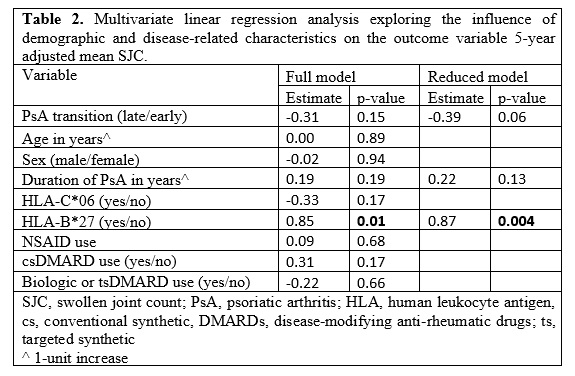
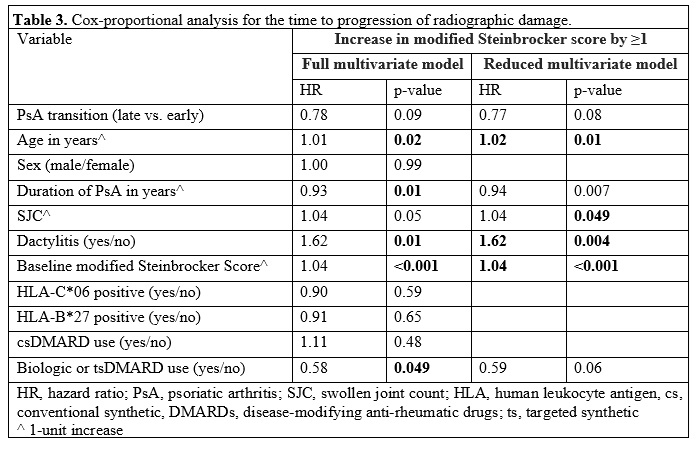
Results: The mean (standard deviation) age at cohort entry of the 702 patients included in the study was 43.6 (13.6) years; 388 (55.3%) were males. 366 (52.1%) patients had an early transition (≤9 years) while 336 (47.9%) had a late transition ( >9 years). In the regression analysis (Table 1), the late transition group was associated with a younger age at the onset of psoriasis (OR 0.93, p< 0.001), older age at the onset of PsA (OR 1.04, p< 0.001), higher body mass index (BMI) (OR 1.03, p=0.01), higher Psoriasis Area Severity Index (PASI) (OR 1.03, p=0.003), and less frequent use of conventional synthetic disease-modifying ant-rheumatic drugs (DMARDs) at baseline (OR 0.70, p=0.04); adjusting for human leukocyte antigen (HLA)-B*27 and/or HLA-C*06, separately or concurrently, did not impact the results. There was a trend for lower disease activity over time and slower progression of radiographic damage with late transition as compared to early transition (Tables 2 and 3).
Notably, for the non-concurrent (538 patients; 76.6%) vs. concurrent (164 patients; 23.4%) disease analysis, we observed a similar pattern of baseline characteristics to that seen in Table 1; concurrent disease was also associated with more frequent dactylitis and axial disease (the latter after adjusting for HLA-B*27 and/or HLA-C*06). There was no significant difference between the two groups with regard to the outcomes, 5-year adjusted mean SJC and time to radiographic progression.
Conclusion: Early and late transitions from psoriasis to PsA are not associated with significant differences in the arthritis-defining features at baseline. However, when followed longitudinally, there is a trend for higher disease activity and faster progression of damage in patients with early transition.
To cite this abstract in AMA style:
Kharouf F, Mehta P, Gao S, Pereira D, Cook R, Gladman D, Chandran V. Does the Time Interval Between the Onset of Psoriasis and Psoriatic Arthritis Impact Disease Presentation and Outcomes? [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/does-the-time-interval-between-the-onset-of-psoriasis-and-psoriatic-arthritis-impact-disease-presentation-and-outcomes/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/does-the-time-interval-between-the-onset-of-psoriasis-and-psoriatic-arthritis-impact-disease-presentation-and-outcomes/