Session Information
Session Type: ACR Plenary Session
Session Time: 11:00AM-12:30PM
Background/Purpose: Elderly-onset RA (EORA) patients (age of
onset>60) are less likely to be treated with biologics even when accounting
for disease activity compared to young-onset RA (YORA) patients (age<60) at
the same age. We hypothesize that this difference is related to an increased
risk of serious infections in EORA vs. YORA patients.
Methods: Participants with RA were followed biannually
from 1998 through 2014 in a large US longitudinal study. Each EORA patient was
matched to 3 YORA patients based on age, sex, and calendar year of study entry,
which required all patients to have age>60. Serious infections were defined
as those requiring hospitalization, intravenous antibiotics, or led to death
within a year after the patient’s last observation. Infections were validated
from hospitalization, physician, and death records. Survival analysis methods
(Cox regression, time to first infection using time-varying covariates and
Andersen-Gill multiple failures model) were applied. Confounders included ethnicity,
comorbidity index, HAQ, pain, education, prednisone use, urban vs. rural home,
previous serious infection, and prior number of DMARDs. DMARD treatments were
grouped using the following hierarchical classification: monotherapy
MTX (reference), none, non-cytotoxic DMARD, cytotoxic DMARD, TNF, and non-TNF
biologic. A risk window of 3 months was considered for all DMARDs except
rituximab within the non-TNF group had 12 months.
Results: A total of 1,865 EORA patients were matched
with 5,595 YORA patients. In both groups, 25% were male and 91% white and a median
age between 65-70. EORA and YORA patients had 4.4 (4.2) and 20.9 (12.6) years
of RA duration, respectively. Self-reported prior infections were 4.1% and 7.1%
for EORA and YORA patients, respectively (P<0.01). There were 1,198 serious
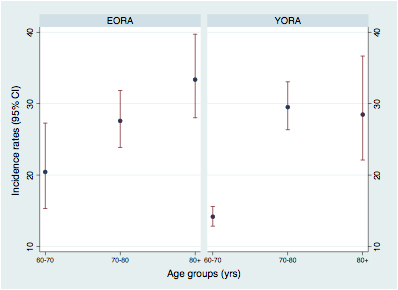
infections, 207 (11.0%) in EORA and 998 (17.8%) in YORA patients. Figure
presents incident rates (first and multiple) by age group. Adjusted for other
confounders, the HR of EORA vs. YORA was 0.84 (0.64-1.11) for first infection
and 1.03 (0.86-1.23) for multiple. Prednisone, cytotoxic DMARDs, and no DMARD
treatment were associated with an increased risk of serious infections as well
as worse HAQ or pain, prior infections, and comorbidities (Table). Sensitivity
analysis stratified patients by decade of age and no differences were found.
Conclusion: We found no increased risk of serious
infections in EORA vs. YORA patients. Our results support providing similar
treatment for EORA patients as done for elderly YORA patients
Figure. Serious infection incidence rates by decade of
age.
Table. Cox regression for time to first infection and
multiple infections.
|
|
Time to first infection
|
Time to multiple infections
|
||
|
|
Haz. Ratio
|
95% CI
|
Haz. Ratio
|
95% CI
|
|
EORA (vs. YORA) |
0.84 |
(0.64 -1.11) |
1.03 |
(0.86 -1.23) |
|
DMARD treatment (Hierar.)
|
ref. monotherapy MTX
|
|
||
|
None
|
1.24 |
(0.98 -1.56) |
1.24 |
(1.06 -1.47) |
|
Non-cytotoxic DMARD*¤
|
0.72 |
(0.56 -0.93) |
0.82 |
(0.69 -0.98) |
|
Cytotoxic DMARD
|
1.04 |
(0.78 -1.39) |
1.14 |
(0.93 -1.40) |
|
TNF biologic
|
0.91 |
(0.72 -1.15) |
0.96 |
(0.81 -1.13) |
|
Non-TNF biologic*¤
|
0.43 |
(0.25 -0.75) |
0.48 |
(0.33 -0.69) |
|
Prednisone*¤ |
2.19 |
(1.88 -2.54) |
2.08 |
(1.87 -2.31) |
|
Male*¤ |
1.37 |
(1.16 -1.62) |
1.42 |
(1.26 -1.60) |
|
Age*¤ |
1.36 |
(1.09 -1.69) |
1.23 |
(1.07 -1.40) |
|
Age-squared*¤ |
1.00 |
(1.00 -1.00) |
1.00 |
(1.00 -1.00) |
|
RA Duration (log yrs)
|
0.97 |
(0.84 -1.11) |
1.07 |
(0.97 -1.19) |
|
Caucasion*¤ |
1.77 |
(1.25 -2.50) |
1.80 |
(1.38 -2.34) |
|
HAQ (0-3)*¤ |
1.43 |
(1.27 -1.61) |
1.47 |
(1.35 -1.59) |
|
Pain (0-10)*¤ |
1.05 |
(1.02 -1.08) |
1.04 |
(1.01 -1.06) |
|
Education (yrs)¤
|
0.98 |
(0.95 -1.01) |
0.97 |
(0.95 -0.99) |
|
Cormorbidity index (0-9)*¤ |
1.18 |
(1.13 -1.24) |
1.19 |
(1.15 -1.23) |
|
# of prior DMARDs (log)*¤ |
1.14 |
(1.03 -1.25) |
1.10 |
(1.04 -1.18) |
|
# of prior biologics (log) |
1.04 |
(0.92 -1.19) |
1.05 |
(0.97 -1.15) |
|
Urban (vs. rural)*¤ |
1.17 |
(1.00 -1.36) |
1.13 |
(1.01 -1.26) |
|
Prior infection¤ |
1.23 |
(0.96 -1.57) |
1.49 |
(1.27 -1.75) |
|
*P<0.01 for time to first infection; ¤P<0.01 for time to multiple infections |
||||
To cite this abstract in AMA style:
Pedro S, Mikuls TR, Michaud K. Does the Risk of Serious Infections Among Elderly RA Patients Differ By Age of Disease Onset? [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/does-the-risk-of-serious-infections-among-elderly-ra-patients-differ-by-age-of-disease-onset/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/does-the-risk-of-serious-infections-among-elderly-ra-patients-differ-by-age-of-disease-onset/