Session Information
Date: Sunday, November 8, 2015
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: The
self-administered comorbidity questionnaire (SCQ) was developed to understand
the impact of 13 common comorbidities on functioning and resource utilisation.
In patients with ankylosing spondylitis, we recently showed that criterion- and
construct validity of the SCQ was good, and improved after removing rheumatic items from the questionnaire
(SpA-SCQ) (1). However, this modification (SpA-SCQ)
does not address uveitis, psoriasis and inflammatory bowel disease,
which are frequently occurring extra-articular manifestations (EAMs) in
spondyloarthritis (SpA), and might have a relevant impact on disease specific
and generic outcomes. The aim of the present study was to assess and compare criterion and construct validity
of the SpA-SCQ and the SpA-SCQ with 3 items representing the EAMs
(“SpA-SCQ-EAM”).
Methods: Data from the CO-MOrbidities in SPA (COMOSPA) study, conducted in 22 countries, were
used. We hypothesised that the criterion validity of the added EAM, assessed by agreement (kappa) between patients’
self-reported and physicians’ confirmed diagnoses of each of the three EAM, was good. For construct validity, we hypothesised that the
SpA-SCQ-EAM would correlate moderate (r>0.30) and somewhat better (r-difference
>0.05) than SpA-SCQ with demographics, physical function (BASFI), work-ability
(WPAI) and health utility (EQ-5D),and that both would have low correlation with
disease activity (ASDAS-CRP). We further hypothesized that the SpA-SCQ(-EAM)
correlated better with these outcomes (but not disease activity) than the rheumatic disease comorbidity index (RDCI).
Results: 3,984 patients
(age 43.6 (SD 13.9) years, 2,588 (65.0%) male, disease duration 8.2 (SD 9.3)
years, of which 2,217/3,067 (72.4%) HLA-B27 positive) contributed to the analyses.
The mean SpA-SCQ was 2.0 (SD 2.8) and the SpA-SCQ-EAM 2.8 (SD 3.3). The
agreement between patient and physician diagnosed EAMs was substantial to
almost perfect (uveitis ĸ=0.81, IBD ĸ=0.74, psoriasis ĸ=0.78),
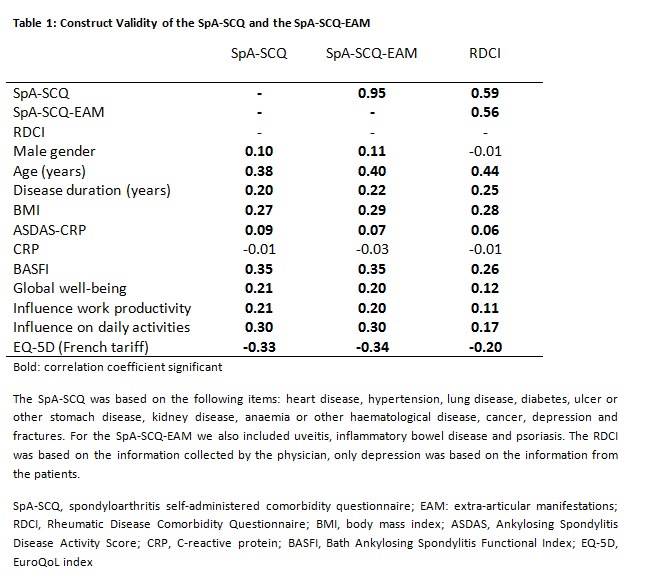
and was not systematically different across countries. Table 1 shows the
correlations between the SpA-SCQ-(EAM) and outcomes, and makes clear that the
hypothesis of a better correlation of the SpA-SCQ-EAM than SpA-SCQ with
outcomes could not be confirmed. On the other hand, both
the SpA-SCQ and the SpA-SCQ-EAM performed better with respect to the correlations
with outcomes than the RDCI (Table 1). Similar results were found for patients
with axial and ‘pure’ peripheral SpA.
Conclusion:
EAMs can be reliably assessed through
self-report by patients with SpA. Notwithstanding, adding the EAMs to the
SpA-SCQ can improve the face validity of this questionnaire. Both the SpA-SCQ
and SpA-SCQ-EAM correlated better with health outcomes than the RDCI in
patients with (axial and peripheral) SpA.
To cite this abstract in AMA style:
Essers I, Stolwijk C, Etcheto A, Molto A, van Den Bosch F, van der Heijde D, Landewé RBM, van Tubergen A, Dougados M, Boonen A. Does the Inclusion of Extra-Articular Manifestations Improve Validity of the Self-Administered Comorbidity Questionnaire Modified for Spondyloarthritis (SpA-SCQ)? Results from ASAS-Comospa [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/does-the-inclusion-of-extra-articular-manifestations-improve-validity-of-the-self-administered-comorbidity-questionnaire-modified-for-spondyloarthritis-spa-scq-results-from-asas-comospa/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/does-the-inclusion-of-extra-articular-manifestations-improve-validity-of-the-self-administered-comorbidity-questionnaire-modified-for-spondyloarthritis-spa-scq-results-from-asas-comospa/