Session Information
Date: Sunday, November 8, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Comorbidities
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Various studies have shown that individuals with Systemic Lupus Erythematosus (SLE) have a higher risk of stroke and cerebrovascular events than the general population. These events represent a significant cause of death in SLE patients. It is however unclear if SLE patients who develop cerebrovascular events have different outcomes compared to stroke patients without SLE. The aim of this study is to compare the outcomes of patients primarily admitted for ischemic stroke with and without a secondary diagnosis of SLE.
Methods: Data were abstracted from the National Inpatient Sample (NIS) 2016 and 2017 Database. This database is the largest collection of inpatient hospitalization data in the United States (U.S). The NIS was searched for hospitalizations for adult patients with ischemic stroke as principal diagnosis with and without SLE as secondary diagnosis using ICD-10 codes. The primary outcome was inpatient mortality. Hospital length of stay (LOS), total hospital charges, odds of receiving tissue plasminogen activator (TPA), and mechanical thrombectomy were secondary outcomes of interest. Multivariate logistic and linear regression analysis was used accordingly to adjust for confounders. Confounders adjusted for include age, sex, Charleston co-morbidity index, and cardiovascular comorbidities. STATA software was used to analyze the data.
Results: There were over 71 million discharges included in the combined 2016 and 2017 NIS database. Out of 525,570 patients with ischemic stroke, 2,280 (0.43%) had SLE. SLE group was younger (58 vs 70 years, P< 0.0001) and had more females (83% vs 50%, P< 0.0001). The adjusted odds ratio (AOR) for inpatient mortality for ischemic stroke with co-existing SLE compared to without co-existing SLE was 0.95 (95% CI 0.58-1.54, P=0.824). Hospitalizations for ischemic stroke with co-existing SLE had higher mean total hospital charges ($80,306 vs $70,157, P=0.019) and less odds of receiving TPA (OR: 0.61, 95% CI 0.41-0.90, P=0.012) compared to those without co-existing SLE.
Conclusion: Patients admitted primarily for ischemic stroke with a secondary diagnosis of SLE had similar inpatient mortality, more total hospital charges, and less likelihood of receiving TPA compared to those without SLE. LOS and odds of receiving mechanical thrombectomy were similar between both groups. Though SLE is known to increase the risk of cerebrovascular events, SLE does not negatively affect outcomes of patients primarily admitted for ischemic stroke based on this large U.S hospital database.
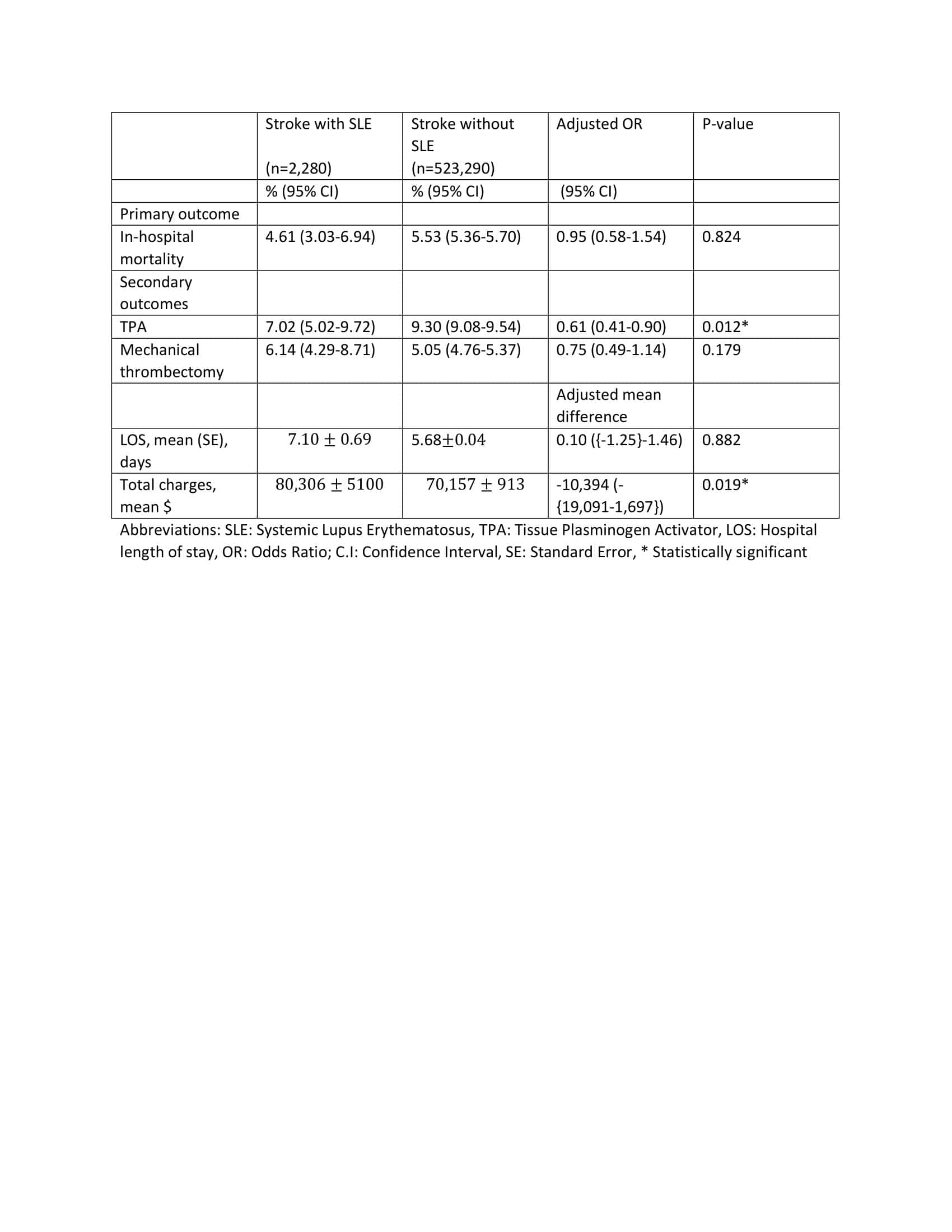 Table 1: Clinical outcomes of ischemic stroke hospitalizations with and without SLE
Table 1: Clinical outcomes of ischemic stroke hospitalizations with and without SLE
To cite this abstract in AMA style:
Edigin E, Eseaton P, Ojemolon P, Manadan A. Does Co-existing Systemic Lupus Erythematosus Affect Outcomes of Hospitalizations for Ischemic Stroke? [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/does-co-existing-systemic-lupus-erythematosus-affect-outcomes-of-hospitalizations-for-ischemic-stroke/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/does-co-existing-systemic-lupus-erythematosus-affect-outcomes-of-hospitalizations-for-ischemic-stroke/
