Session Information
Date: Tuesday, November 14, 2023
Title: Abstracts: Patient Outcomes, Preferences, & Attitudes II: Patient Experience
Session Type: Abstract Session
Session Time: 4:00PM-5:30PM
Background/Purpose: The COVID-19 pandemic affected medication adherence in patients with autoimmune disease (AD) due to their fear of contracting COVID-19, financial hardship, and medication shortage. We compared adherence to disease-modifying antirheumatic drugs (DMARDs) before, during, and after the COVID-19 pandemic among patients with AD and evaluated whether adherence affected the risk of contracting COVID-19.
Methods: This retrospective study included patients aged ≥18 years in a large integrated healthcare system during 2019-2021, who had ICD-coded diagnoses of AD and ≥2 DMARDs prescriptions dispensed by outpatient pharmacy. DMARDs were classified as synthetic (sDMARDs) or biologic (bDMARDs). Medication adherence was measured by the Medication Possession Ratio (MPR), with adherence defined as MPR ≥80%. Adherence during the pre-pandemic year (March 19, 2019 to March 18, 2020), pandemic year (March 19, 2020 to March 18, 2021), and vaccine era (March 19, 2021 to September 18, 2021) were compared using the Wilcoxon test. Multivariable logistic regression was used to examine the association of treatment adherence and risk of COVID-19, reporting odds ratios (OR) and 95% confidence intervals (CI), adjusted for age, sex, race and ethnicity, primary language, smoking, weight category, and presence of other chronic health conditions.
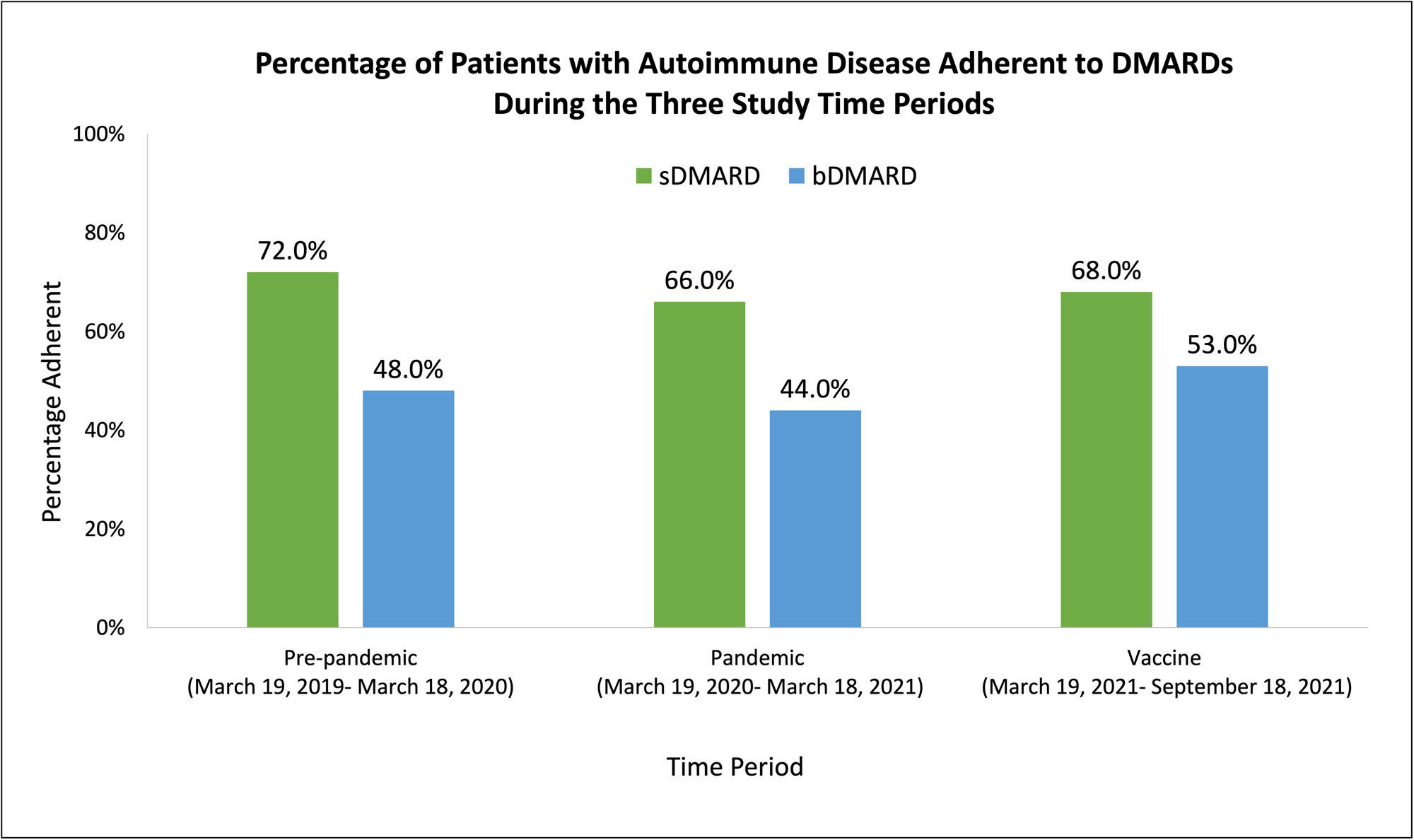
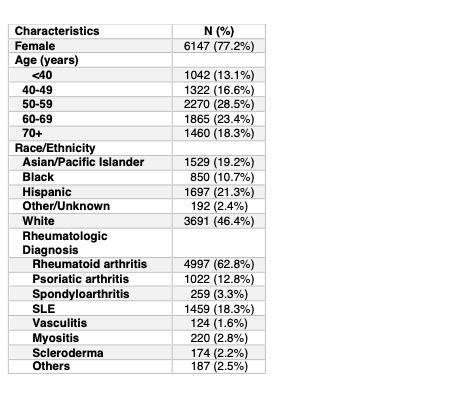
Results: The cohort included 7959 patients with AD; 77.2% were female, 46.4% were White, 21.3% Hispanic, 19.2% Asian/Pacific Islander (PI), and 10.7% Black race. The most common AD diagnoses were rheumatoid arthritis (62.8%), psoriatic arthritis (12.8%), and lupus (18.3%). The most commonly prescribed sDMARDs were methotrexate (51.5%), hydroxychloroquine (45.8%), and leflunomide (17.3%), while the most commonly prescribed bDMARDs were tofacitinib (14.3%), TNF inhibitors (7.7%), and abatacept (2.9%). The majority were receiving sDMARD monotherapy (69.8%), followed by combination sDMARD and bDMARD therapy (24.4%), bDMARD monotherapy (3.6%), and sDMARD triple therapy (3.6%). Of patients prescribed sDMARDs, 72% were adherent in the pre-pandemic year, 66% in the pandemic year, and 68% in the vaccine era. Of patients prescribed bDMARDs, 48% , 44%, and 53% were adherent in the pre-pandemic, pandemic, and vaccine era. Differences in adherence between the time periods were statistically significant (p< 0.01) for both sDMARDs and bDMARDs. Adherence to sDMARDs was associated with lower risk of COVID-19 infection (OR 0.73, 95% CI 0.60-0.88), adjusting for covariates. Similar findings were seen for adherence to bDMARDs (OR 0.56, 95% CI 0.34-0.94).
Conclusion: In a large population of patients with AD, medication adherence, particularly to bDMARDs, was low even pre-pandemic and decreased further during the pandemic, but subsequently increased in the vaccine era. Medication adherence was associated with lower risk of COVID-19 infection. These findings support efforts to reduce barriers to medication adherence, including addressing patient concerns regarding infection risk. Future studies should examine whether there is an association between poor medication adherence and severity of COVID-19 infection and outcomes.
To cite this abstract in AMA style:
Selvam T, Peterman K, Haghshenas A, Liu L. DMARD Adherence During the COVID-19 Pandemic and Association with Risk of COVID-19 Infection [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/dmard-adherence-during-the-covid-19-pandemic-and-association-with-risk-of-covid-19-infection/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/dmard-adherence-during-the-covid-19-pandemic-and-association-with-risk-of-covid-19-infection/