Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: The gastrointestinal tract (GIT) is commonly involved in SSc with up to 98% of patients reporting GIT manifestations. Small intestinal bacterial overgrowth (SIBO) is more prevalent in patients with SSc than the general population, but little is known about the relationship between SIBO and SSc. To better understand the gut microbiota of patients with SSc, we compared fecal bacterial compositions of SSc patients to a healthy cohort. We additionally examined differences in the gut microbiota of SSc patients with or without SIBO and inflammatory seromarkers.
Methods: Adults with SSc (ACR/EULAR criteria) were assessed as having SIBO (SIBO+) or no SIBO (SIBO-) using an H2/CH4 breath test. GIT symptoms were assessed using the UCLA SCTC GIT 2.0 questionnaire. To analyze microbiome composition, DNA was isolated from fecal samples of individual patients, and 16S rRNA gene was amplified and sequenced with Illumina technique. The gut microbiota of patients with SSc was compared to controls with no history of autoimmune disease and GIT symptoms. Additional analyses were conducted according to the presence/absence of anti-centromere antibody (ACA) and antibodies against topoisomerase I (Scl-70) in patients with SSc. Microbiome Β-diversity of SIBO+ and SIBO- patients was compared using Bray Curtis dissimilarity matrix.
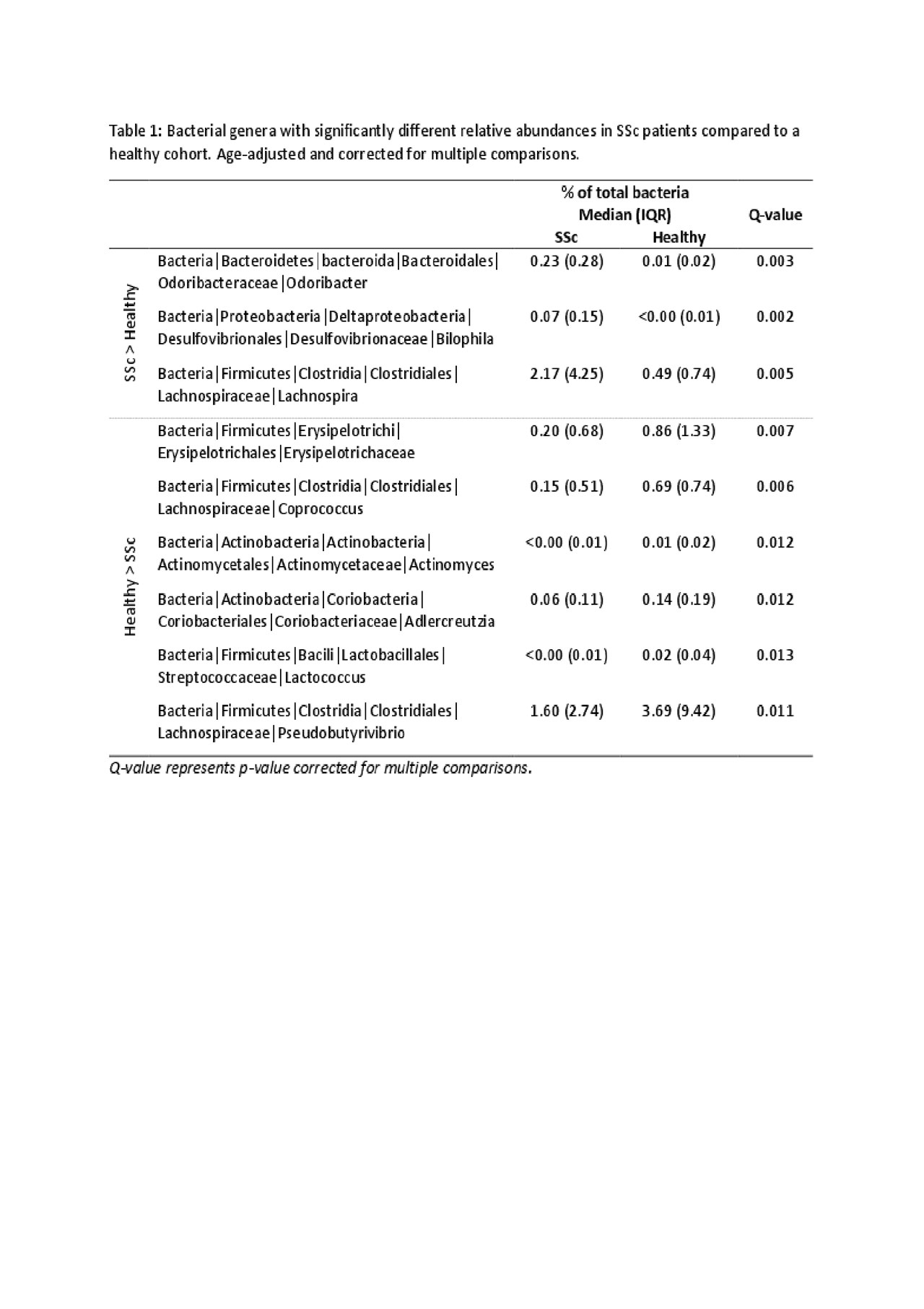
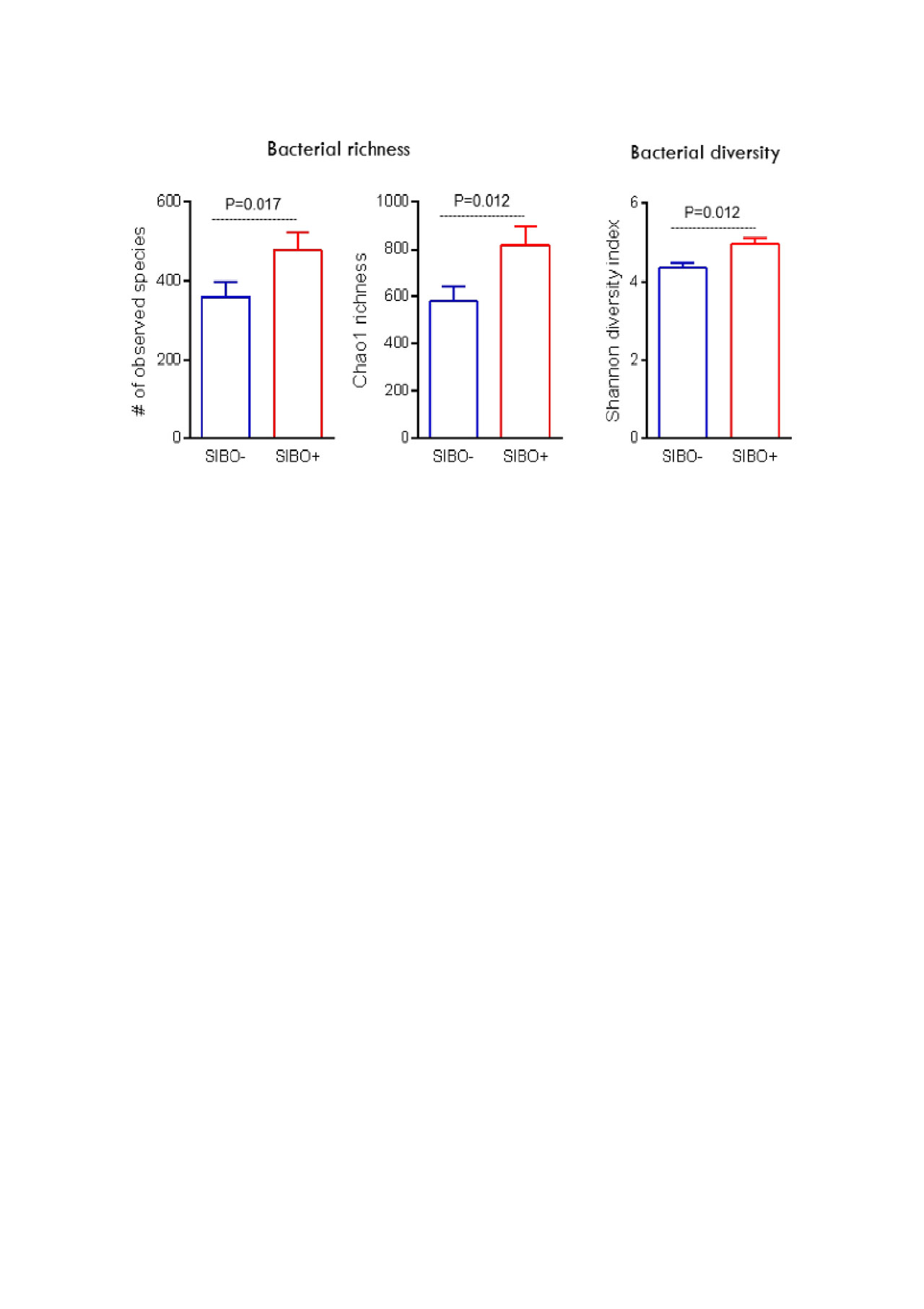
Results: Of 25 SSc patients (mean (SD) age = 56.4 (11.2) years, 96% female), 13 (52%) tested SIBO+, 19 (76%) ACA+, 4 (16%) anti-Scl70+ and 2 (8%) were seronegative. The healthy cohort consisted of 20 participants (mean (SD) age = 33.1 (13.5) years, 70% female). After correcting for multiple comparisons and the effect of age differences, the composition of microbiota in SSc patients was significantly different from healthy controls; notably, patients with SSc had increased abundance of Odoribacter, Bilophila and Lachnospira species (p< 0.05) and decreased abundance of Erysipelotrichaceae, Adlercreutzia, Lactococcus, and Pseudobutyrivibrio species (p< 0.05) (Table 1). Compared to SIBO- patients, SIBO+ patients had significantly higher bacterial richness (Chao1 and observed species) and diversity (Shannon diversity index) (Figure 1). Although SIBO+ and SIBO- patients did not have significantly different microbiome compositions, SIBO+ ACA+ SSc patients had significantly higher abundance of Rikenellaceae species in comparison to SIBO- ACA+ SSc patients. SIBO- patients reported significantly more reflux [SIBO+ mean SD 0.59 (0.56), SIBO- 1.31 (0.59), p< 0.01], while SIBO+ patients experienced more (but p >0.05) soilage [SIBO+ 0.62 (0.87), SIBO- 0.18 (0.40)] and diarrhea [SIBO+ 0.62 (0.46), SIBO- 0.36 (0.45)].
Conclusion: The current study is the first to examine the relationship between SIBO and SSc on a bacterial level and found notable differences between the microbiota composition of SIBO+ and SIBO- SSc patients. These differences in gut microbiota appeared to affect the presentation of GIT symptoms. The increased microbiota richness and diversity of SIBO+ patients may exacerbate inflammatory disease activity, and the effects of SIBO on SSc progression and response to treatment warrant further exploration.
To cite this abstract in AMA style:
Zou H, De Palma G, Bercik P, Verdu E, Beattie K, Larche M. Distinct Characteristics of the Gut Microbiome of Patients with Systemic Sclerosis and Small Intestinal Bacterial Overgrowth [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/distinct-characteristics-of-the-gut-microbiome-of-patients-with-systemic-sclerosis-and-small-intestinal-bacterial-overgrowth/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/distinct-characteristics-of-the-gut-microbiome-of-patients-with-systemic-sclerosis-and-small-intestinal-bacterial-overgrowth/