Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: A shortage of Rheumatologists has led to gaps in inflammatory arthritis (IA) care in Canada. Amplified in rural-remote communities, the number of Rheumatologists practicing rurally cannot be meaningfully increased. Alternate care strategies must be adopted. The economic impact of a shared-care Telerheumatology model, utilizing a community-embedded Advanced Clinician Practitioner in Arthritis Care (ACPAC)-ERP and an urban-based Rheumatologist, is described in terms of the estimated travel cost-savings (distance not traveled) for both patients and the healthcare system.
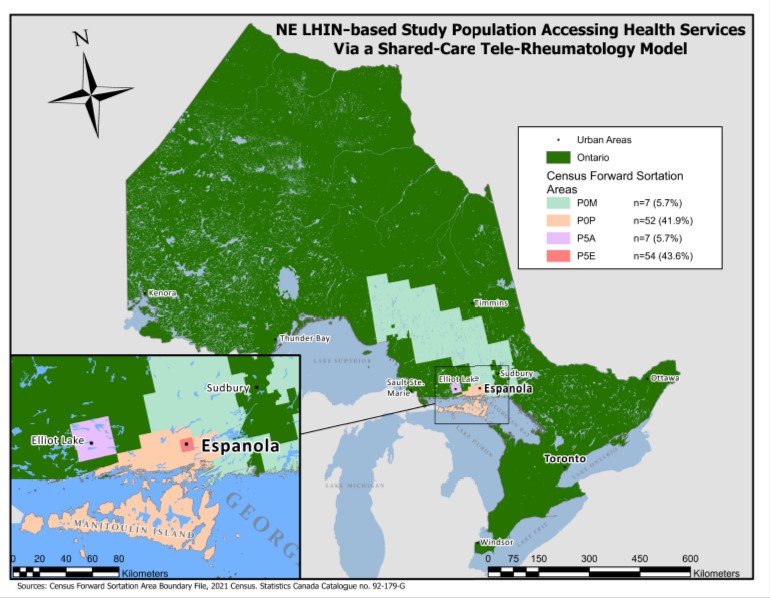
Methods: A Rheumatologist and an ACPAC-ERP located 463 kilometers distally, established a monthly half-day Hub-and-Spoke-Telerheumatology clinic to care for patients with suspected IA, triaged by the ACPAC-ERP. Subsequent collaborative visits occurred with the Rheumatologist (Hub-St. Michael’s Hospital, Toronto) attending virtually. Geospatial information for individual patients was obtained using regional postal codes collected through demographic data. Calculations of hypothetical distances between these locations and St. Michael’s Hospital were based on the most efficient and cost-effective driving route utilizing Google Maps©. Aggregate data were used to calculate distances not travelled due to the virtual care delivery model. An estimation of further cost-savings of this Telerheumatology shared model of care was based on Ministry of Health (MOH) travel grants that would have been reimbursed to these patients should they have traveled for in-person care.
Results: Data from 124 patients seen between January 2013-January 2022 were collected: 98.0% (n=496/504 visits) were virtual. An estimated 493,470 km of patient-related travel was avoided (basedon 494 Telerheumatology visits). The loci where more than 5 patients resided is represented in Figure 1.A theoretical estimate of the MOH travel grant cost was $276,428, calculated based on the total number of patient visits that would have been incurred should these patients have been followed by the Rheumatologist in-person.
Conclusion: Half of a million kilometers (493,470 km) of travel was avoided for the patients involved in this Telerheumatology study, significantly reducing the carbon footprint and environmental impact by not travelling to access specialist rheumatology care. The estimated $276,428 cost-savings in this study represents a minimal base fiscal value of the ACPAC-trained ERP working within a Telerheumatology model of care. Other indirect costs need to be further captured in a more robust economic analysis. There is a compelling fiscal argument to support scaling-upof this model to deliver comprehensive and cost-effective virtual rheumatologic care in underserved communities provincially and beyond.
To cite this abstract in AMA style:
Steiman A, Murdoch J, Shupak R, Inrig T, Lundon K. Distance Not Travelled in a Tele-Rheumatology Shared Care Model: Leveraging the Expertise of an Advanced Clinician Practitioner in Arthritis Care (ACPAC)-trained Extended Role Practitioner (ERP) in Rural-remote Ontario [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/distance-not-travelled-in-a-tele-rheumatology-shared-care-model-leveraging-the-expertise-of-an-advanced-clinician-practitioner-in-arthritis-care-acpac-trained-extended-role-practitioner-erp-in-ru/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/distance-not-travelled-in-a-tele-rheumatology-shared-care-model-leveraging-the-expertise-of-an-advanced-clinician-practitioner-in-arthritis-care-acpac-trained-extended-role-practitioner-erp-in-ru/