Session Information
Date: Sunday, November 17, 2024
Title: RA – Treatment Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Despite the significant therapeutic benefits of various disease modifying anti-rheumatic drugs (DMARDs) in RA, concerns remain regarding their safety, particularly their potential impact on cancer risk and outcomes. RA itself is associated with an increased risk of certain malignancies, including lung cancer, which is a leading cause of cancer-related mortality worldwide. Very little is known regarding use of DMARDs after lung cancer diagnosis and their association with mortality in patients with RA. We aimed to evaluate the association between duration of DMARD use post-lung cancer diagnosis in patients with RA and mortality at 1 year.
Methods: This retrospective cohort study utilized data from the national Veterans Affairs (VA) Corporate Data Warehouse (CDW), from 2002 to 2022. Patients with RA were identified using 2 International Classification of Disease (ICD) codes within 7-365 days, accompanied by DMARD prescription fill within 1 year. Patients who developed lung cancer during follow up using data from the VA Oncology Raw Domain were identified. Patients were excluded if they had a lung cancer diagnosis recorded prior to (prevalent cancer) or within 6 months of RA diagnosis (likely paraneoplastic arthritis). Main exposure was duration of DMARD use, categorized as 0-3 months, 3-6 months and >6months use. To avoid immortal time bias, DMARD use was characterized as a time-varying exposure. The primary outcome was one-year mortality following lung cancer diagnosis. Demographic and clinical characteristics, including age, sex, marital status, race, ethnicity, region, rurality, tobacco use, cancer stage (AJCC), and histology type, were recorded. Kaplan-Meier survival analysis was used to compare survival rates among the three groups. Cox proportional hazards models were performed adjusting for above confounders.
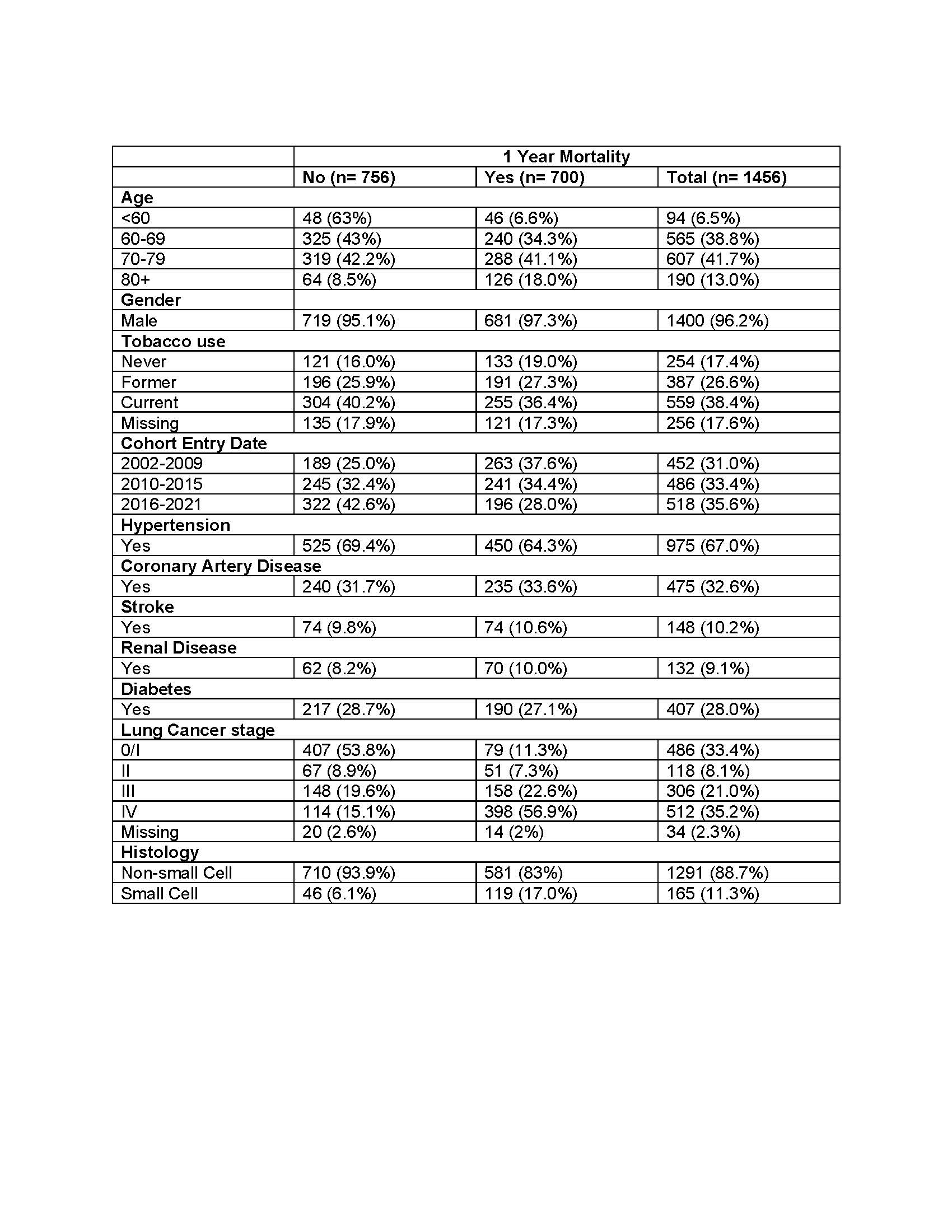
Results: We identified 1,456 patients with RA and incident lung cancer. The one-year mortality rate was 48.1% (700/1,456). The cohort had a mean age of 70 years, predominantly male (96.2%), and mostly white (79.5%) (Table 1). Tobacco use was prevalent, with 38.4% being current smokers, and 12.6% former smokers.
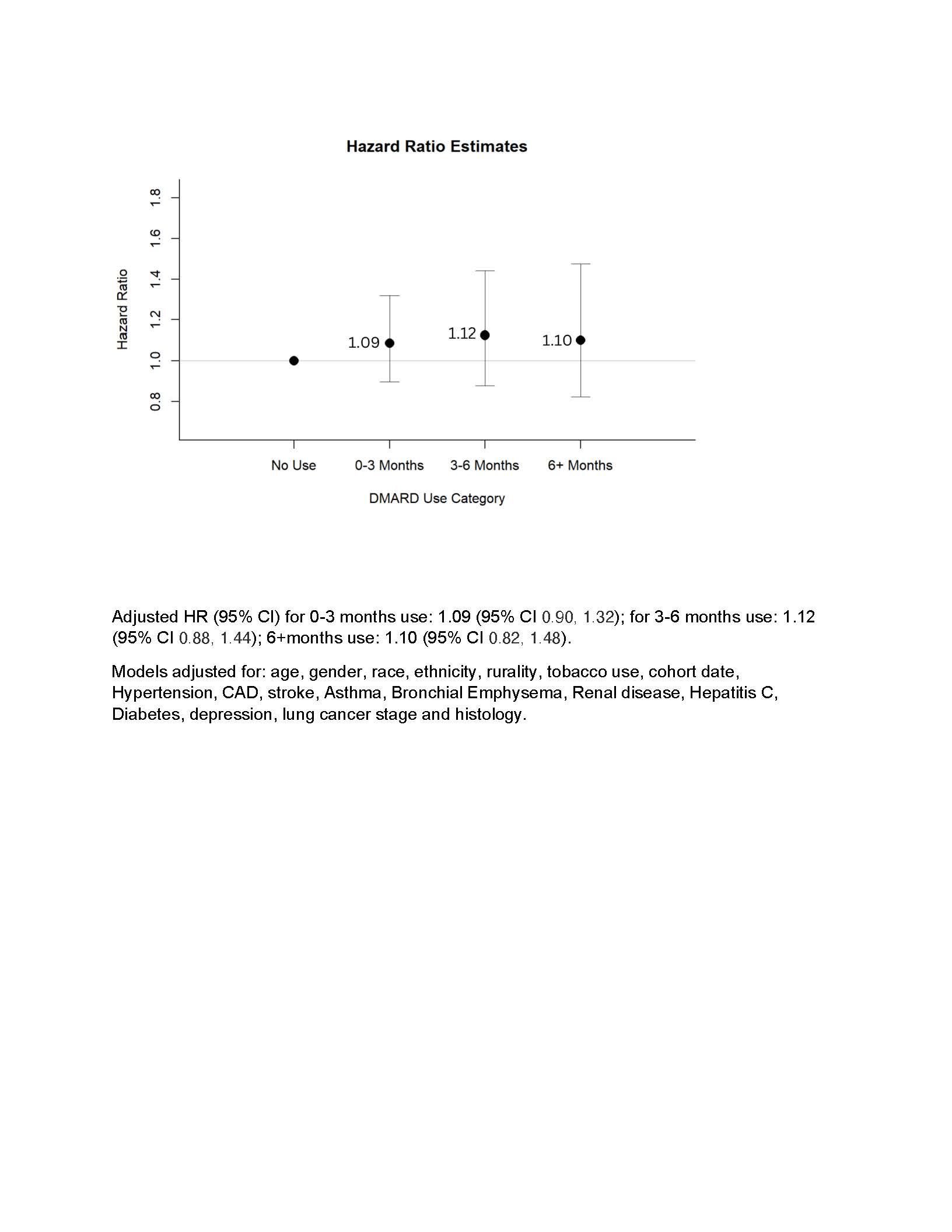
Unadjusted hazard ratios (HR) for use of a DMARD begun within the first-year post lung cancer diagnosis showed a trend towards reduced mortality risk with longer duration of use: 1.19 (95% CI: 0.98, 1.45) for 0-3 months, 1.06 (95% CI: 0.83, 1.36) for 3-6 months, and 0.78 (95% CI: 0.59, 1.03) for 6+ months. Adjusted hazard ratios showed similar trends: HR for 0-3 months use 1.09 (95% CI 0.90, 1.32) and for 6+ months use was 1.10 (95% CI 0.82, 1.48), although they were not statistically significant (Figure 1).
Conclusion: Use of DMARDs for RA post lung cancer diagnosis was not associated with increased mortality in our study. Further studies are necessary to confirm these results as well as evaluate associations with longer-term mortality. These results can help guide point-of-care discussions in clinical practice.
To cite this abstract in AMA style:
Nandakumar V, Baraff A, Peterson A, Smith N, Barton J, O'Hare A, Li C, Weiss N, Singh N. Disease Modifying Anti-rheumatic Drug Use and Association with Survival in Patients with Rheumatoid Arthritis and Newly Diagnosed Lung Cancer [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/disease-modifying-anti-rheumatic-drug-use-and-association-with-survival-in-patients-with-rheumatoid-arthritis-and-newly-diagnosed-lung-cancer/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/disease-modifying-anti-rheumatic-drug-use-and-association-with-survival-in-patients-with-rheumatoid-arthritis-and-newly-diagnosed-lung-cancer/