Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: During pregnancy, patients with rheumatoid arthritis (RA) can experience flares that might influence pregnancy outcomes. We aimed at assessing disease course during pregnancy and identifying possible risk factors of disease flares.
Methods: Data about RA patients prospectively followed in a pregnancy clinic were retrospectively collected before conception and during each trimester (T). Clinical characteristics, disease activity (DAS28-CRP3), medication use, and pregnancy outcomes were analysed. Flare was defined by an increase of DAS28-CRP3 >0.6 if the DAS28-CRP3 was >3.2 and by an increase of DAS28-CRP3 >1.2 if the DAS28-CRP3 was ≤3.2.
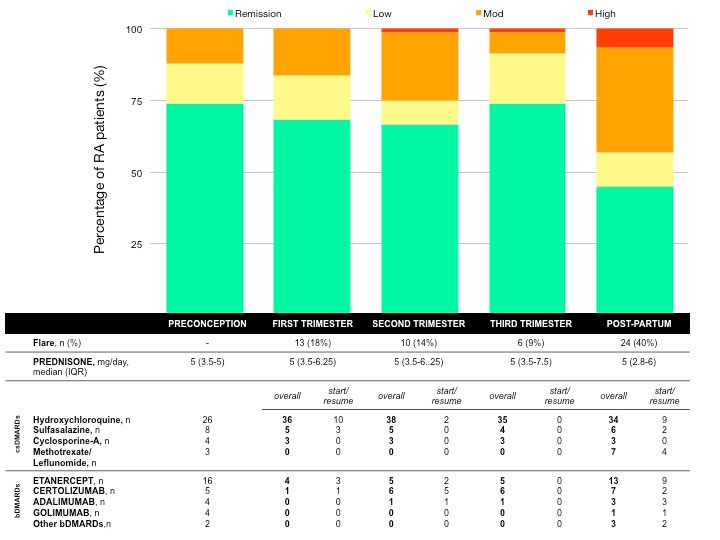
Results: Among 83 pregnancies (median age 35-IQR 30-38; median disease duration 66 months, IQR 36-156; ACPA+ 62.3%%, RF+ 60.2%) in 64 RA patients enrolled between 2010 and 2018, 8 pregnancies ended with early miscarriages, 1 with intrauterine foetal death and 1 with ectopic pregnancy. The remaining 73 pregnancies in 63 patients were analysed. Before conception, 54(74%) patients were in remission, 10 (14%) had low disease activity and 9 (12%) moderate disease activity (Fig.1). During pregnancy, a flare occurred in 27 (37%) patients (13 in T1, 10 in T2, 6 in T3; 2 patients had >1 flare). Flares during pregnancy were associated with the discontinuation of bDMARDs at positive pregnancy test (55% of patients with flare vs 30% of patients with no flare, p=0.034 OR 2.857, 95%CI 1.112-8.323). Flares during the course of pregnancy were also associated with a previous use of >1 bDMARDs (33% of patients with flare vs 10% of patients with no flare, p=0.019, OR 4.1, 95%CI 1.204-13.966). Fig.1 reports the use of drugs during each trimester and post-partum period (presented as overall use and start/resume of single drugs). Particularly, patients who stopped bDMARDs at the beginning of pregnancy resumed it during 2nd-3rd trimester (12/29, 41.4%) or after delivery (13/29, 44.8%). Twenty-four live births (33%) were complicated (9 preterm deliveries, of which 3 < 34weeks; 12 premature rupture of membranes (PROM), 5 at term and 7 preterm; 10 “small for gestational age” newborns). Preterm pregnancies were characterised by higher values of CRP and DAS28-CRP3 at T1 compared with pregnancies at term (10 (5-11) vs 3 (2.5-5) p=0.01 and 4.2 (1.9-4.5) vs 1.9 (1.7-2.6) p=0.01, respectively). Preterm deliveries were associated with the occurrence of flare (flare 27% vs no-flare 7%, p=0.034, OR 4.625, 95%CI 1.027-20.829).
Conclusion: In a cohort of prospectively-followed pregnancies, 37% of RA patients experienced at least one flare during pregnancy despite the majority of the patients were in remission prior to conception. There was a 3-fold-increased chance of flare in patients who were on bDMARDs (and stopped the treatment early in pregnancy) as compared with bDMARDs-naïve patients. Patients with more aggressive RA (use of bDMARDs, especially if >1) may get benefit from continuing treatment beyond conception to ensure control of maternal disease and better pregnancy outcomes.
To cite this abstract in AMA style:
Gerardi M, Andreoli L, García-Fernández A, Bazzani C, FILIPPINI M, FREDI M, GORLA R, Lazzaroni M, Nalli C, TAGLIETTI M, ZATTI S, LOJACONO A, Franceschini F, Tincani A. Disease Flares of Rheumatoid Arthritis During Pregnancy: What Is the Impact of Stopping bDMARDs at the Beginning of Pregnancy? [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/disease-flares-of-rheumatoid-arthritis-during-pregnancy-what-is-the-impact-of-stopping-bdmards-at-the-beginning-of-pregnancy/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/disease-flares-of-rheumatoid-arthritis-during-pregnancy-what-is-the-impact-of-stopping-bdmards-at-the-beginning-of-pregnancy/