Session Information
Date: Sunday, November 10, 2019
Title: 3S078: RA – Diagnosis, Manifestations, & Outcomes I: Pulmonary & Other Comorbidities (839–844)
Session Type: ACR Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Rheumatoid arthritis is associated with a higher risk of diabetes mellitus (DM) and cardiovascular disease. While disproportional obesity and visceral fat accumulation may contribute to a higher incidence of DM, the systemic inflammatory disease may directly lead to insulin resistance and promote the development of cardiometabolic disease. Our aim was to evaluate associations between disease activity (including evaluation of specific cytokines and chemokines) among veterans with RA and determine independent associations with incident DM incidence in a longitudinal cohort.
Methods: Participants were enrollees in a multicenter, longitudinal observational cohort of US veterans with RA. Baseline demographics, comorbidities, body mass index (BMI), ACPA status, disease activity (DAS28-CRP), and active therapies were derived from query of the electronic medical record and registry data. Therapies and disease activity were assessed as time-varying covariates in initial models. Seventeen cytokines and chemokines were measured in banked serum obtained at the time of enrollment in a subset of partiipants using a bead-based multiplex assay. Cytokine/chemokine values were log-adjusted and standardized (all values are per 1 SD). Incident DM was defined as the presence of a new diagnosis code at any time in follow-up (following at least 12 months of follow up without a code). Multivariable Cox proportional hazards models evaluated associations between clinical factors and incident DM. Independent associations between specific cytokines and chemokines were assessed adjusting for age, sex, race, smoking, and medication use at baseline.
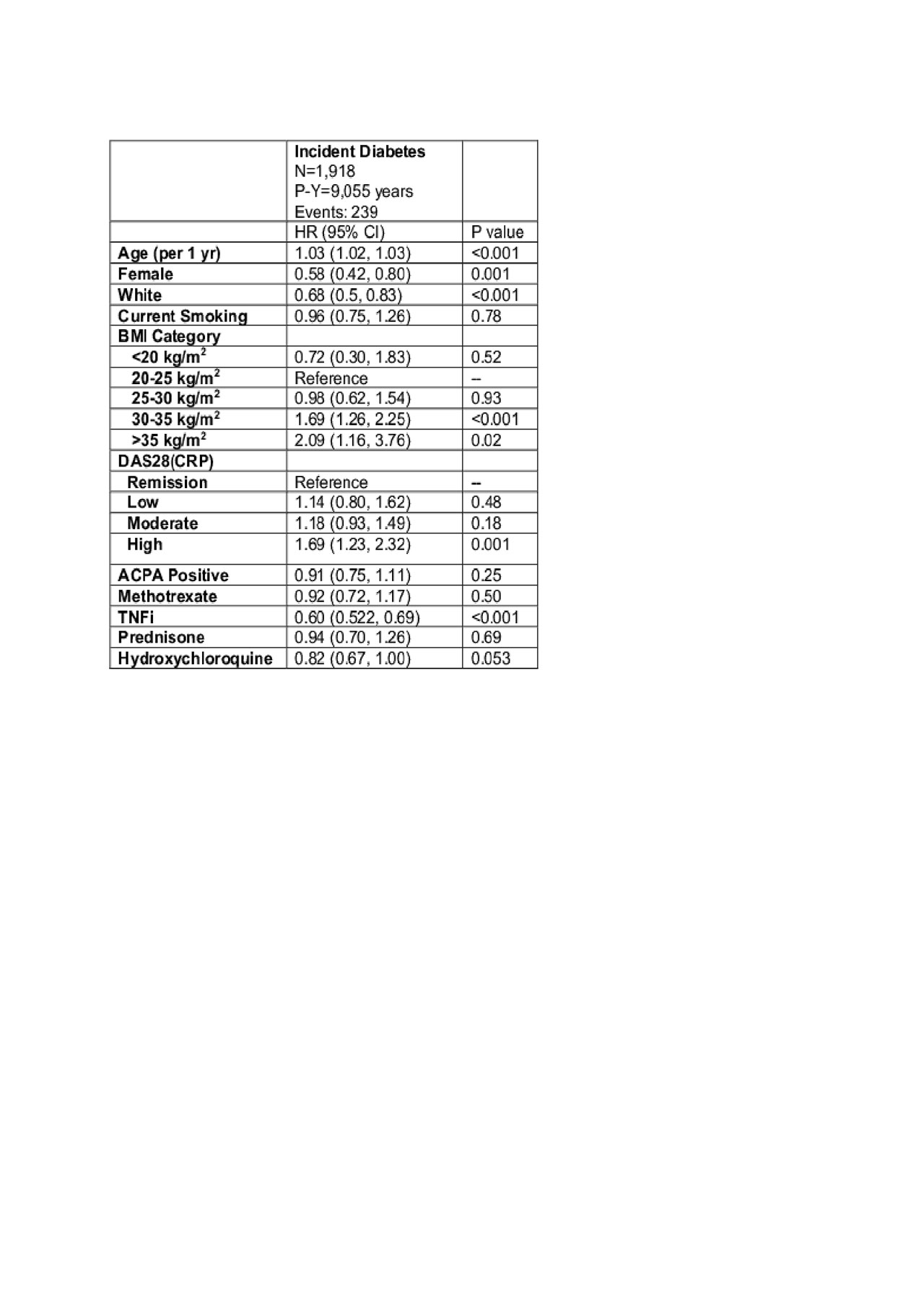
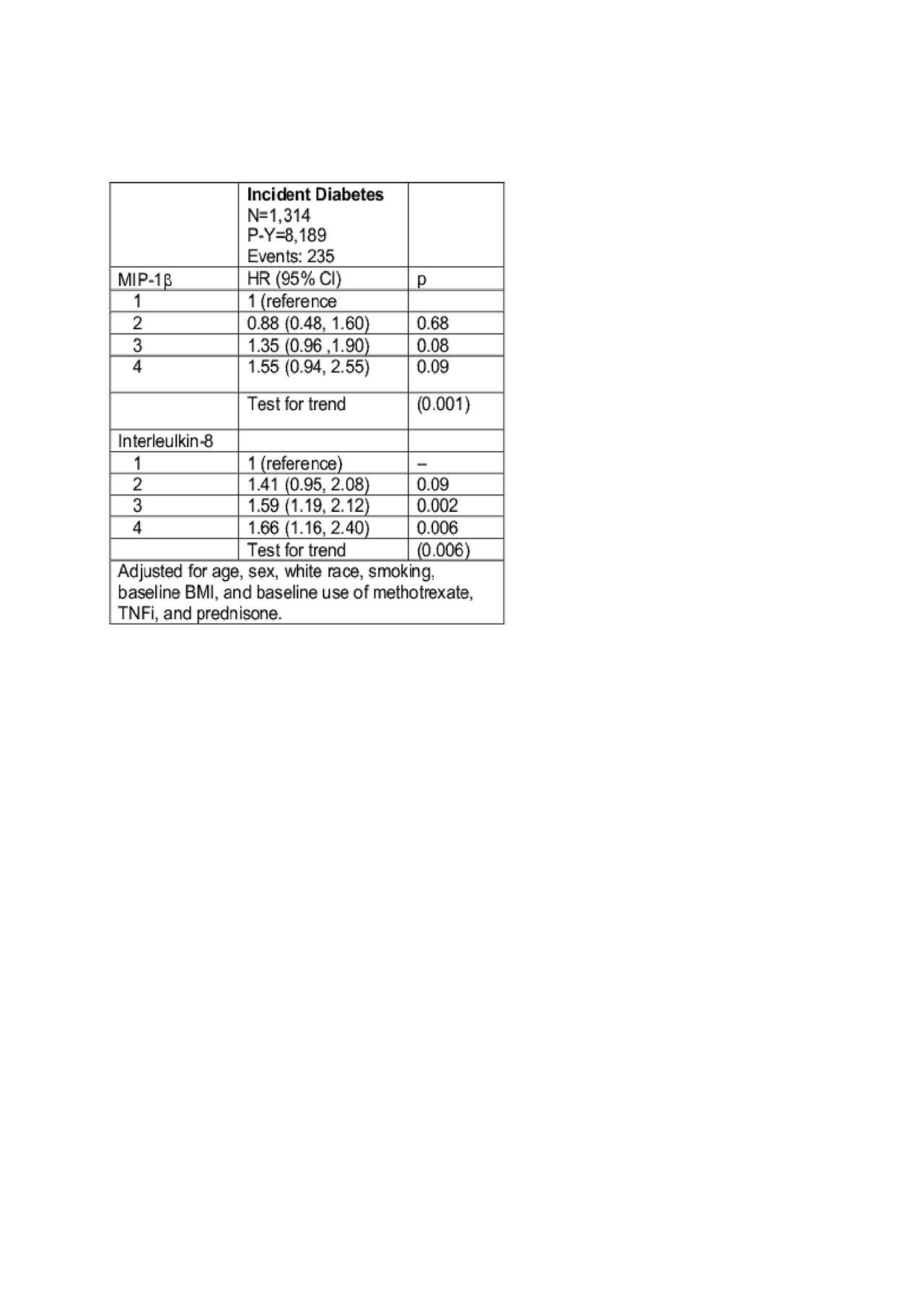
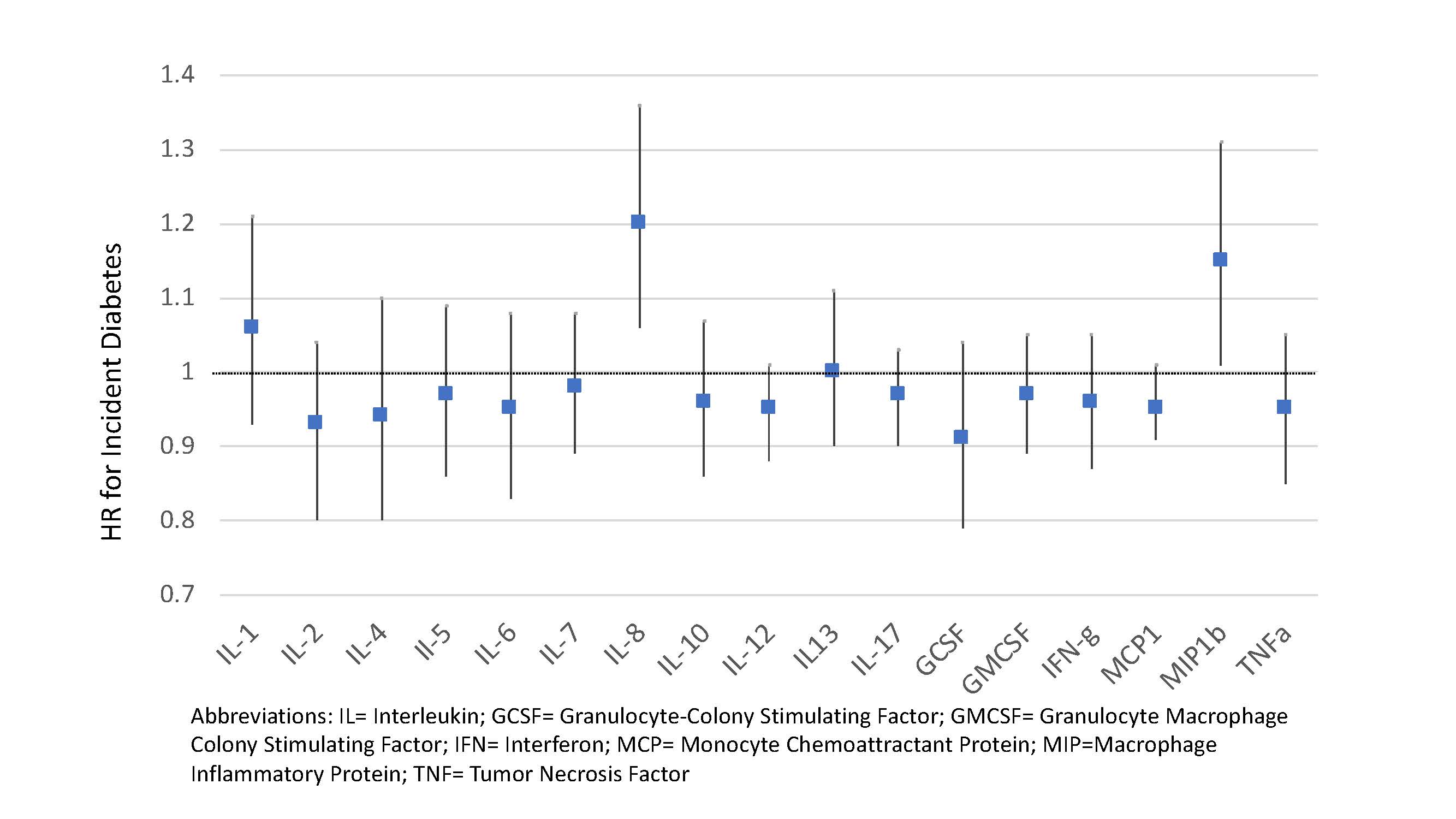
Results: Among 1,918 RA patients without prevalent DM, there were 239 cases of incident DM over 9,055 person-years of follow-up. Patients with high disease activity, obese BMI, older age, male sex, and non-white race were at the greatest risk for incident DM (Table 1). Those using TNFi were at significantly lower risk. In models adjusting for demographics, smoking, and baseline medication use, two chemokines evaluated were significantly associated with the incidence of DM (per 1 SD). These were Macrophage Inhibitory Protein (MIP)-1b [HR 1.20 (95% CI 1.04, 1.39) p=0.01] and Interleukin(IL)-8 [HR 1.16 (95% CI 1.02, 1.33) p=0.02] (Figure). Higher quartiles of MIP-1b and IL-8 were associated with incident DM in a dose-dependent manner (Table 2). These associations were not attenuated with adjustment for DAS28-CRP.
Conclusion: Older age, male sex, higher disease activity, greater BMI, and elevated levels of the chemokines MIP-1b and IL-8 are associated with incident DM in veterans with RA. Notably, levels of IL-1, TNF-a, and IL-6 were not significantly associated with incident DM in this population although TNFi use was predictive of future DM. Future study may help to determine if other targeted treatments in at-risk individuals could help to prevent the development of DM in patients with RA.
To cite this abstract in AMA style:
Baker J, England B, George M, Cannon G, Mikuls T. Disease Activity, Cytokine Profiles, and the Risk of Incident Diabetes in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/disease-activity-cytokine-profiles-and-the-risk-of-incident-diabetes-in-rheumatoid-arthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/disease-activity-cytokine-profiles-and-the-risk-of-incident-diabetes-in-rheumatoid-arthritis/