Session Information
Date: Monday, November 18, 2024
Title: Abstracts: SpA Including PsA – Diagnosis, Manifestations, & Outcomes II
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: Diagnostic delays in psoriatic arthritis (PsA) among psoriasis patients are common due to under recognition by referring providers. Previous studies show that a PsA screening survey in clinic settings identifies patients suitable for rheumatology referral and administering the survey directly to patients via email or mail increases rheumatology evaluations. However, the appropriateness of referrals generated through the direct-to-patient (D2P) survey method remains unknown. This study aimed to evaluate the appropriateness of rheumatology evaluations for patients who screened positive via the D2P method and to assess treatment patterns following their initial rheumatologic evaluation.
Methods: Patients with psoriasis but no PsA diagnosis codes in electronic health records at the University of Utah received the Psoriasis Epidemiology Screening Tool (PEST) Survey by email and mail on 04/28/23. Those screening positive were directed to schedule a rheumatology appointment. We extracted patient demographics, clinical evaluations, and treatment outcomes. A referral was deemed appropriate if patients had: (1) physician-confirmed psoriasis; (2) no previous rheumatologist encounter; and (3) PsA diagnosis or symptoms, examination findings, or test results warranting further workup or a rheumatology follow-up.
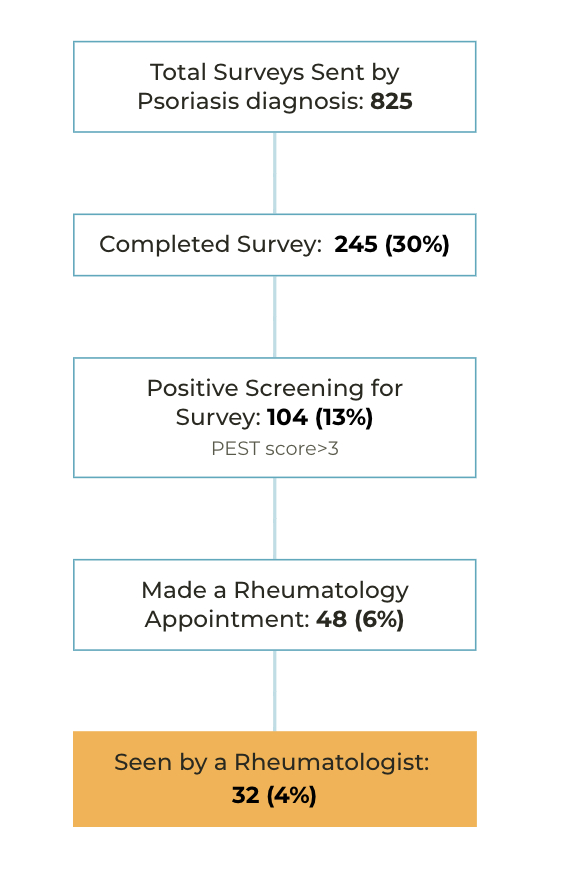
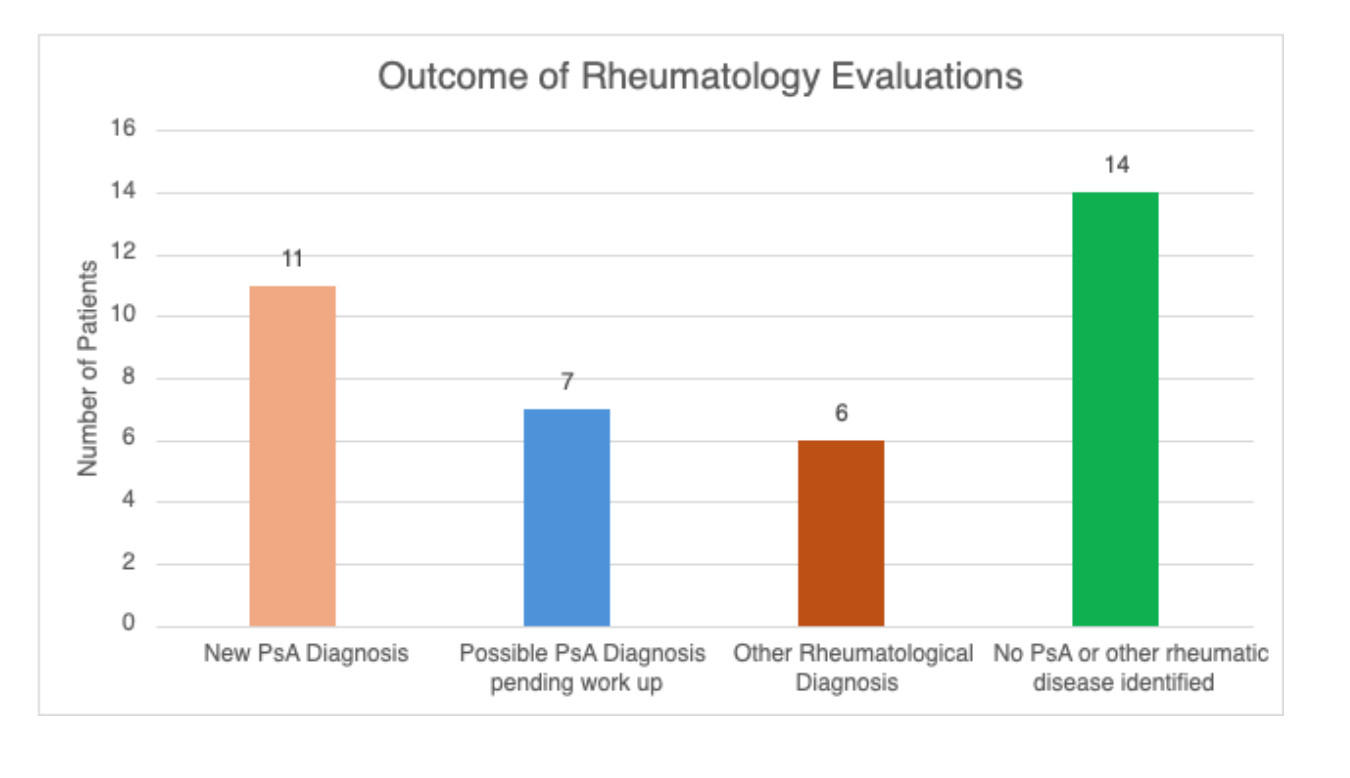
Results: Surveys were sent to 825 patients, 245 (30%) completed the survey. A positive screening was positive in 104 (13%) patients, 32 (4%) were seen by a rheumatologist by June 2024 (Figure 1). It took about 4 months from receipt of the survey by patients to see a rheumatologist. The majority were Caucasian (84%) and female (53%), with a mean age of 54.9 years. Thirty patients (94%) had confirmed psoriasis,11 (34%) were diagnosed with PsA, and 7 (22%) were pending PsA investigation. Other rheumatologic diagnoses identified in 6 (19%) patients (Figure 2).
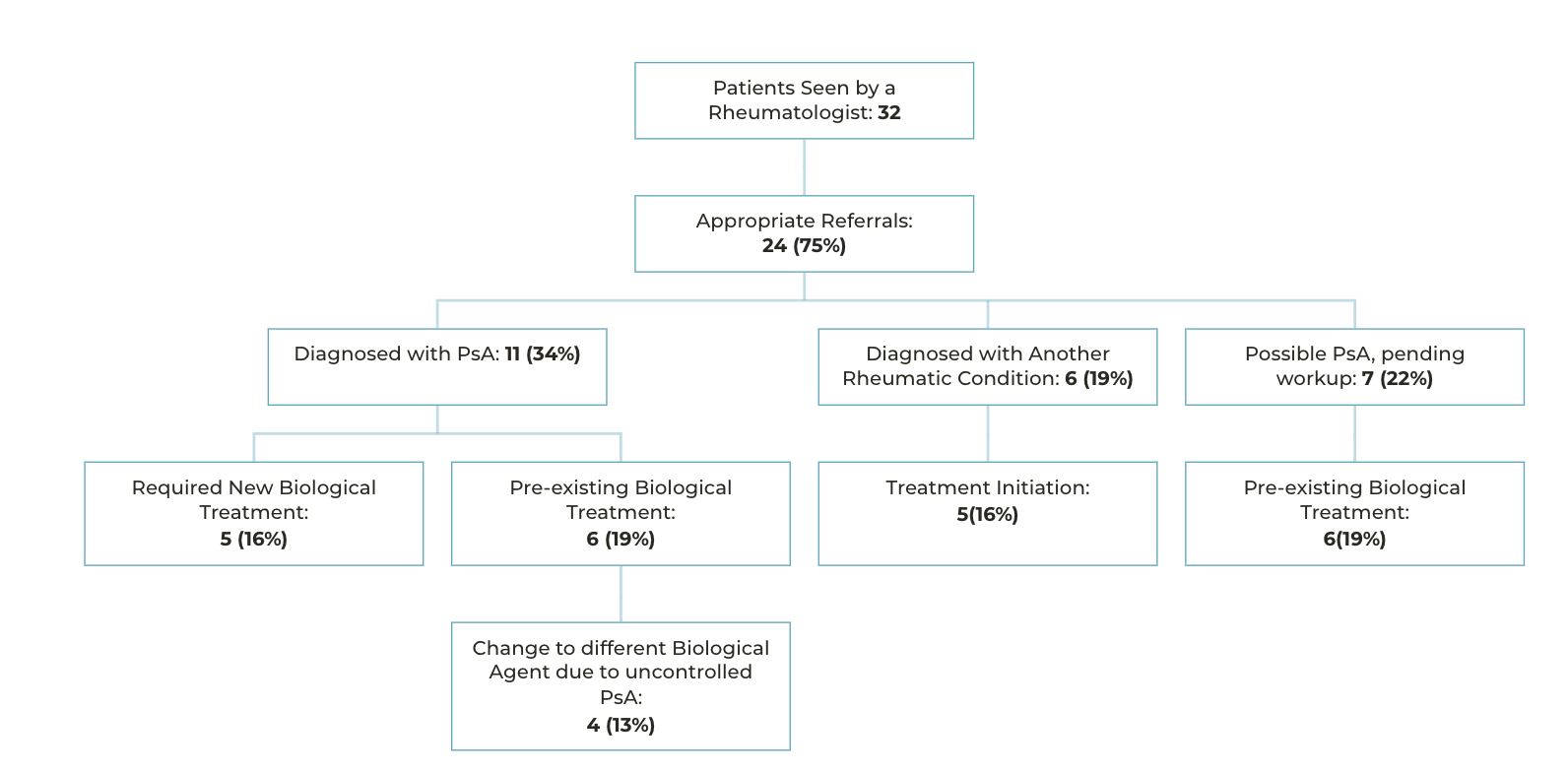
Rheumatology Referrals were deemed appropriate in 24 (75%) patients due to a new diagnosis of PsA or possible PsA and/or another new rheumatic diagnosis. Among the newly diagnosed PsA patients, 5/11 patients required treatment initiation for PsA and the rest 6/11 were already on biologic treatment for psoriasis. However, 4/6 PsA patients on existing biologics were recommended to switch agents due to inadequate PsA control. Patients diagnosed with another new rheumatic condition 5/6 patients required treatment initiation. Among patients with unclear PsA diagnosis, 6/7 were already on biologics for psoriasis (Figure 3). Return rheumatology visits were recommended for 23 (72%) patients.
Conclusion: The D2P survey screening effectively identified patients appropriate for rheumatology evaluation, with one-third receiving a new PsA diagnosis. Additional patients benefited from new diagnoses of other rheumatic diseases mimicking PsA. Rheumatology evaluations led to significant treatment changes (44%) and recommendations for follow-up care, demonstrating the D2P approach’s impact on patient outcomes.
To cite this abstract in AMA style:
Alexander S, Pei S, Penmetsa G, Reddy S, Scher J, Ogdie A, Walsh J. Direct to Patient Screening for Psoriatic Arthritis in Patients with Psoriasis: Appropriateness of Rheumatology Referrals and Treatment Outcomes [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/direct-to-patient-screening-for-psoriatic-arthritis-in-patients-with-psoriasis-appropriateness-of-rheumatology-referrals-and-treatment-outcomes/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/direct-to-patient-screening-for-psoriatic-arthritis-in-patients-with-psoriasis-appropriateness-of-rheumatology-referrals-and-treatment-outcomes/