Session Information
Date: Sunday, November 13, 2022
Title: Abstracts: Vasculitis – Non-ANCA-Associated and Related Disorders I
Session Type: Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Giant cell arteritis (GCA) requires rapid diagnostic work up and start of treatment to prevent severe complications. The temporal artery biopsy as a gold standard in diagnosis is debatable, as results can take up to two weeks and can be false negative. Imaging techniques are increasingly used because they generate fast results, are less invasive and have a high sensitivity [1]. However, a direct comparison between different imaging modalities in patients with suspected GCA has never been studied. This pilot study aims to directly compare the diagnostic value of ultrasound (US), [18F]fluorodeoxyglucose-positron emission tomography/computed tomography (FDG-PET/CT) and magnetic resonance imaging (MRI) with each other in patients suspected of GCA.
Methods: Patients were recruited from the prospective GET (GCA early in Twente) cohort study (Hospital Group Twente, the Netherlands) and underwent US, FDG-PET/CT and MRI within five working days after initial diagnostic work-up. In the GET cohort, demographic and clinical characteristics of patients with suspected GCA are collected over five years. To avoid circularity, the clinical diagnosis after six months follow-up made by an independent expert panel blinded for imaging results was defined as the reference diagnosis. This reference diagnosis was used to calculate sensitivity, specificity, negative and positive predictive values. Subanalyses regarding cranial or extracranial artery involvement were performed.
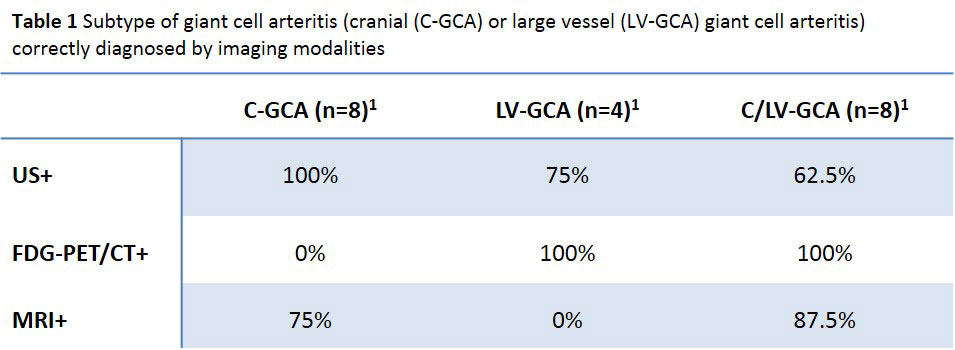
Results: In total, 42 patients with suspected GCA were included. Mean age was 70.7 years (SD 7.7) and 61.9% were female. The expert panel classified 23 patients as GCA after six months follow-up, of whom 95.7% met the revised ACR criteria for GCA. Specificity was 100% for US, FDG-PET/CT and MRI. Sensitivity was 69.6% for US, 52.2% for FDG-PET/CT and 56.5% for MRI (Figure 1). FDG-PET/CT results were positive for GCA in all patients with extracranial artery involvement (n=12), while US and MRI performed more optimal for isolated cranial artery involvement (n=8) (100% and 75% respectively) (Table 1).
Conclusion: The diagnostic value of US, FDG-PET/CT and MRI was comparable with high specificity and moderate sensitivity. FDG-PET/CT performed best in diagnosing extracranial artery involvement while US and MRI performed better for isolated cranial artery involvement. Diagnostic choices should be made considering availability of (state-of-the-art) equipment, operator experience, costs and suspected subtype. As US is non-invasive and allows quick visualization, this can be performed as a first test conform EULAR recommendations [1]. However, with high pre-test probability and inconclusive or negative results, further testing is required based on suspected subtypes.
[1] Dejaco C, Ramiro S, Duftner C, Besson FL, Bley TA, Blockmans D, Brouwer E, Cimmino MA, Clark E, Dasgupta B, Diamantopoulos AP, Direskeneli H, Iagnocco A, Klink T, Neill L, Ponte C, Salvarani C, Slart RHJA, Whitlock M, Schmidt WA. EULAR recommendations for the use of imaging in large vessel vasculitis in clinical practice. Ann Rheum Dis. 2018 May;77(5):636-643.
To cite this abstract in AMA style:
van Nieuwland M, Vermeer M, Colin E, Wagenaar N, Vijlbrief O, van Zandwijk J, Slart R, Koffijberg H, Groot Jebbink E, Brouwer E, Boumans D, Alves C. Direct Comparison of Ultrasound, [18F]Fluorodeoxyglucose-Positron Emission Tomography/Computed Tomography and Magnetic Resonance Imaging: Early Diagnostics in Patients Suspected of Giant Cell Arteritis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/direct-comparison-of-ultrasound-18ffluorodeoxyglucose-positron-emission-tomography-computed-tomography-and-magnetic-resonance-imaging-early-diagnostics-in-patients-suspected-of-giant-cell-arteriti/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/direct-comparison-of-ultrasound-18ffluorodeoxyglucose-positron-emission-tomography-computed-tomography-and-magnetic-resonance-imaging-early-diagnostics-in-patients-suspected-of-giant-cell-arteriti/