Session Information
Date: Tuesday, November 9, 2021
Title: Vasculitis – Non-ANCA-Associated & Related Disorders Poster II (1862–1888)
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Establishing the diagnosis of Primary central nervous system vasculitis CNSV is challenging. In this study we aimed to investigate distinguishing primary CNSV compared to non-inflammatory intracranial vasculopathy using features in clinical presentation and blood and cerebrospinal fluid (CSF) markers.
Methods: We evaluated all cases enrolled in CNS vasculopathy registry ( 2012- present ) which include patients with CNSV and other vasculopathies that mimics CNSV. Final diagnoses was verified with the last follow up. Final diagnosis of primary CNSV was based on criteria proposed by Calabrese and Mallek namely (1) the presence of an unexplained neurologic deficit after thorough clinical and laboratory evaluation, (2) documentation by cerebral angiography and/or tissue examination of an arteritic process within the central nervous system, and (3) no evidence of a systemic vasculitis or any other condition to which the angiographic or pathologic features could be secondary. In cases without evidence of histological confirmation, the diagnosis of CNSV was made according to the clinical pictures, MRI abnormalities, cerebral vascular imaging, and the presence of inflammatory CSF profiles and absolute certainty of the diagnosis that lead to therapeutic trial. Infectious vasculopathy, reversible cerebral vasoconstriction syndrome, systemic inflammatory disease, and cardio-embolic disease were excluded (Table 1). Clinical features on first presentation such as gender, ethnicity, clinical presentation, past medical history, and medications in addition to serum and CSF findings were investigated for their ability to predict the final diagnosis. CSF pleocytosis was defined as CSF white blood cell count ≥ 5 cells/µL and elevated CSF protein > 45 mg/dL.
Results: A total of 206 patients were identified with definite final diagnosis. 36 patients with CNSV and 26 with non-inflammatory vasculopathies (large vessel atherosclerotic disease, small vessel disease, intracranial dissection, and amyloid vasculopathy) were included. Demographics, clinical presentation, and comorbidities in two groups were not significantly different with the exception higher prevalence of male gender and language deficits in CNSV group and higher prevalence of transient ischemic attack and hyperlipidemia in the past medical history of non-inflammatory vasculopathy group (Table 2). A logistic regression model was evaluated with the top 3 features identified in descending order included CSF pleocytosis (coefficient: 1.682), past medical history of hyperlipidemia (coefficient: -0.638), and seizure at presentation (coefficient: 0.478). The model predicted CNSV in validation cohort with sensitivity of 69% and specificity of 76%. This model was then cross-validated and was able to predict CNSV with AUC 0.81, sensitivity 69.44% and specificity 75.86%. The calibration plot for this model is demonstrated in Figure 1.
Conclusion: In this study, we demonstrated that differentiating inflammatory form non-inflammatory CNS vasculopathy can be enhanced using a simple logistic regression model based on patient’s past medical history, clinical presentation, and CSF profile using a logistic regression model.
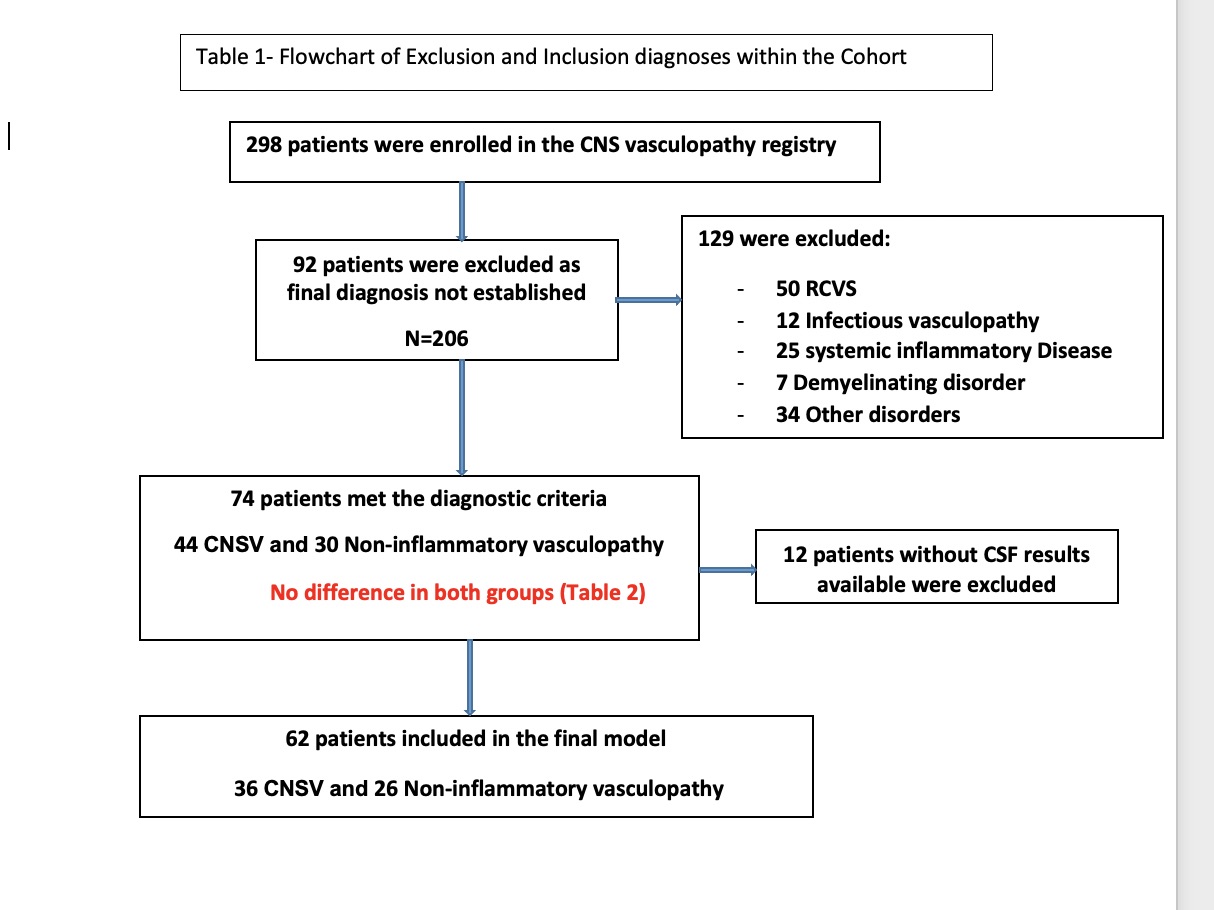 Table_1. Flowchart of Inclusion and ExclusionDiagnoses within the Cohort
Table_1. Flowchart of Inclusion and ExclusionDiagnoses within the Cohort
 Table 2- Comparison of CNSV vs Non -inflammatory vasculopathies
Table 2- Comparison of CNSV vs Non -inflammatory vasculopathies
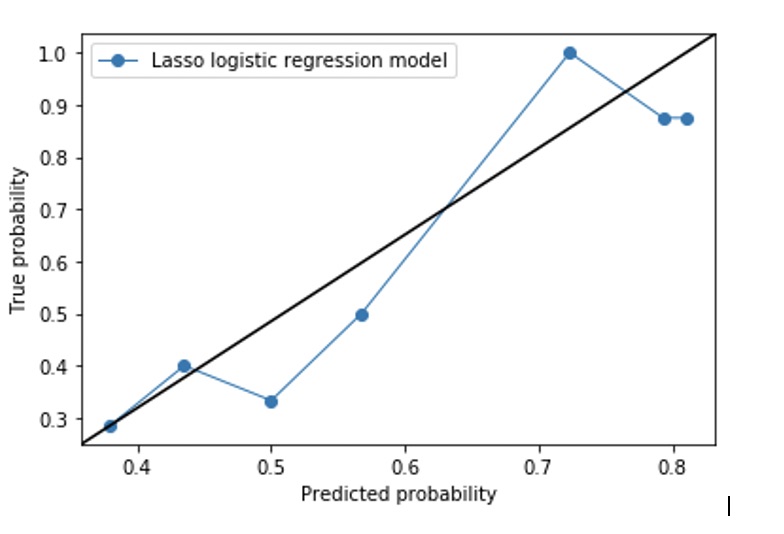 Figure1- Logistic regression model
Figure1- Logistic regression model
To cite this abstract in AMA style:
Amin M, Shimoyama T, Uchino K, Calabrese L, Hajj-Ali R. Differentiating Primary Central Nervous System Vasculitis from Non-inflammatory Intracranial Vasculopathy [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/differentiating-primary-central-nervous-system-vasculitis-from-non-inflammatory-intracranial-vasculopathy/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/differentiating-primary-central-nervous-system-vasculitis-from-non-inflammatory-intracranial-vasculopathy/
