Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: ANCA associated vasculitis (AAV) is a severe autoimmune disorder with substantial morbidity and mortality. Establishing the diagnosis might be challenging due to the existence of noteworthy mimickers, most notably infective endocarditis (IE) and drug-induced AAV. We aimed to identify differences in initial labs, serologies, clinical manifestations, and histopathology findings with the goal recognizing diagnostic clues that can raise suspicion for a secondary process.
Methods: A retrospective chart review was conducted on patients with glomerulonephritis (GN) secondary to IE, drug-induced AAV and primary AAV, from January 1, 2008, to January 1, 2024. Patients were filtered using SNOMED clinical terms of vasculitis and GN and any positive ANCA test. GN was defined histologically via biopsy or clinically by elevated creatinine and new onset hematuria with active urinary sediment. IE diagnosis was established by modified Duke Criteria or positive PCR on removed valve. Primary and drug induced AAV diagnosis were established by vasculitis specialist. Blood counts, and serologies were collected prior to treatment. Statistical analysis included the use of Kruskal-Wallis test for continuous variables and Chi-square test for categorical variables.
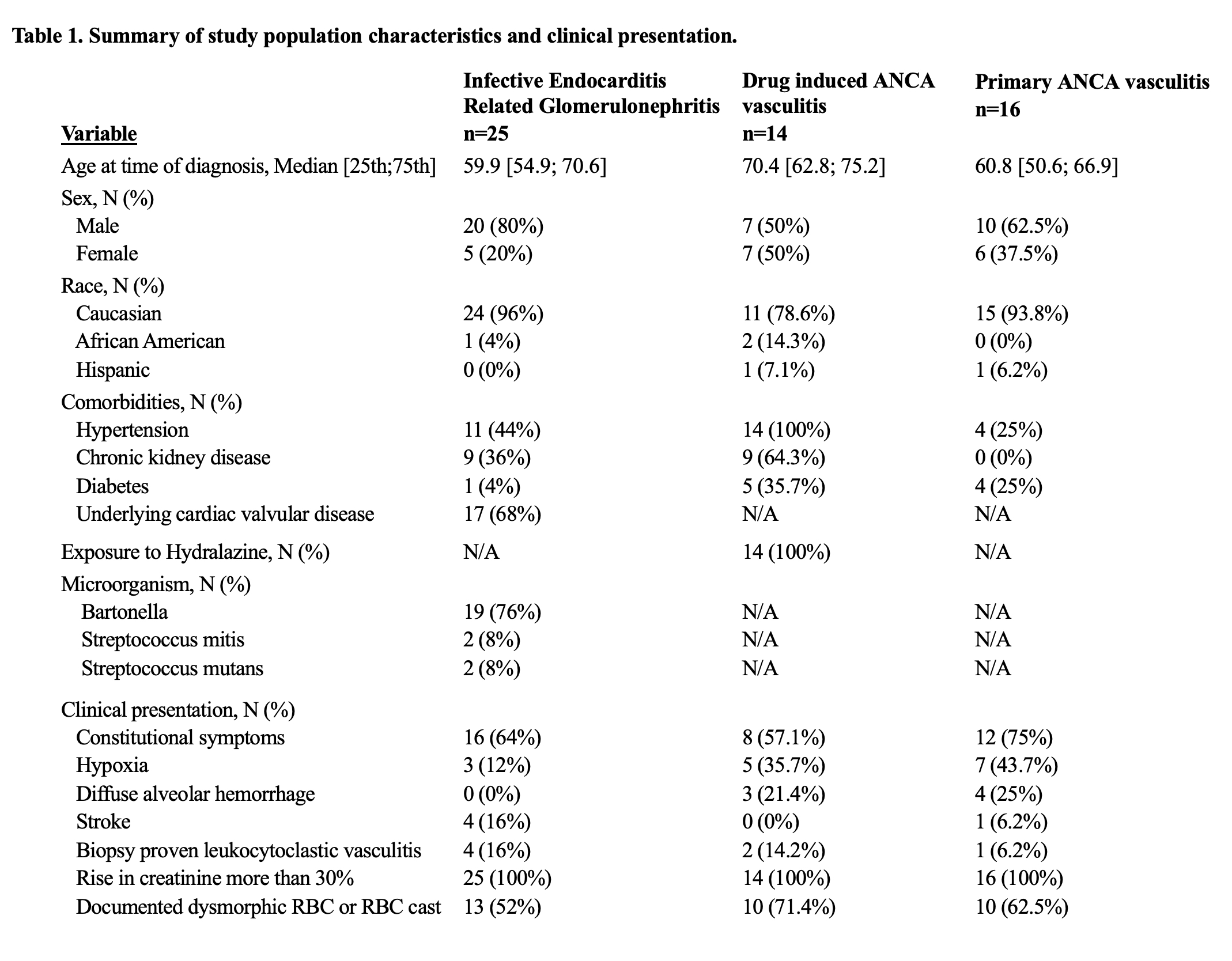
Results: There were 25 patients with IE related GN, 14 with drug-induced AAV, and 16 with primary AAV (Table 1). Median age at diagnosis was 59.9, 70.4, and 60.8 years, respectively. Bartonella was the most common microorganism (76%) in the IE-related GN group. All drug-induced AAV cases were linked to hydralazine.
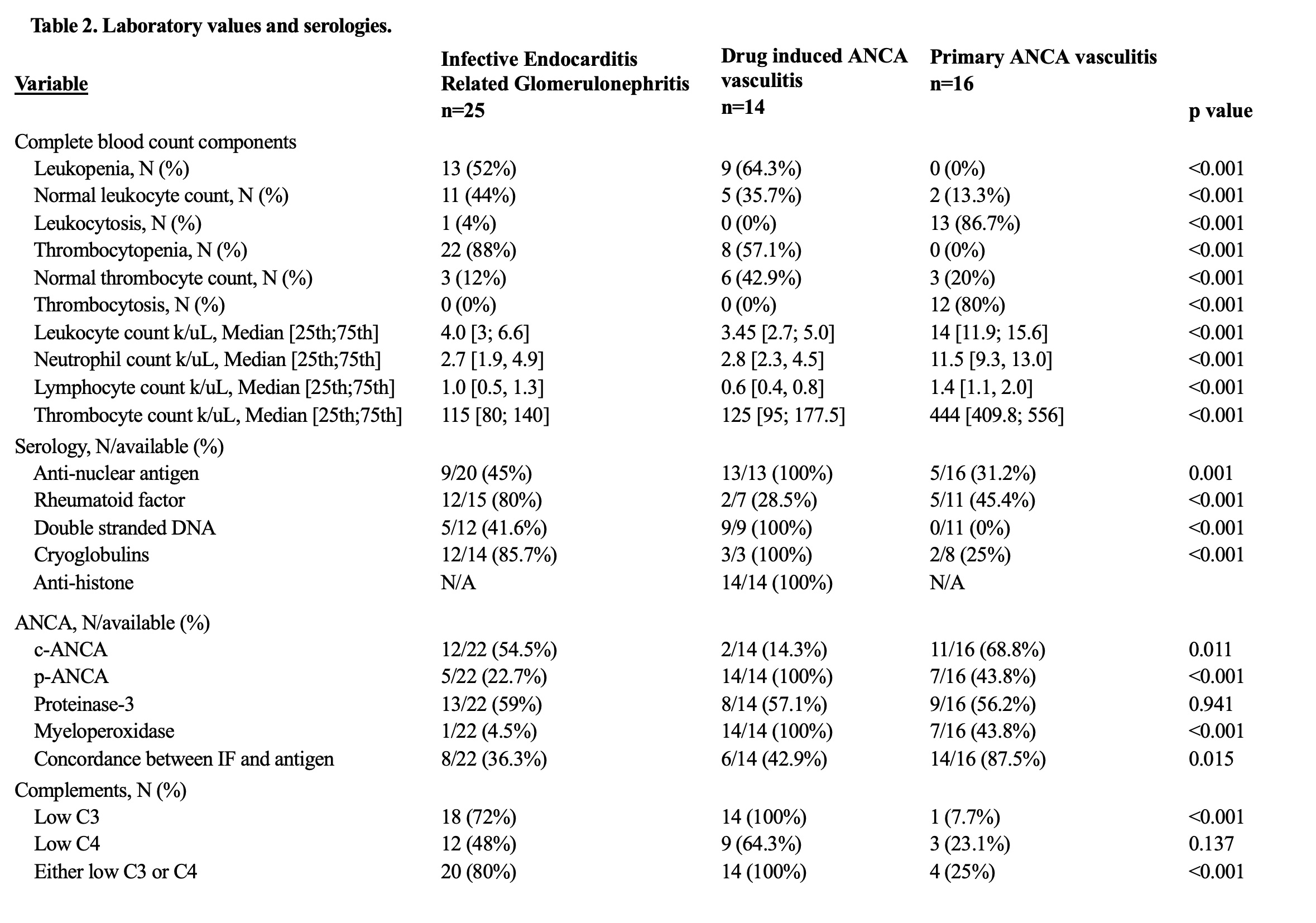
Baseline labs and serologies are detailed in Table 2. Initial blood counts showed that IE-related GN and drug-induced AAV patients commonly presented with leukopenia (52% and 64.3%, respectively) and thrombocytopenia (88% and 57.1%, respectively). Primary AAV cases frequently presented with leukocytosis (86.7%) and thrombocytosis (80%). Median leukocyte, neutrophil, lymphocyte, and platelet counts at diagnosis were higher in primary AAV compared to other groups (p< 0.001). Low complements found in 80% of IE-related GN and 100% of drug-induced AAV cases (p< 0.001). Myeloperoxidase was positive in all drug-induced AAV, and 43.8% of primary AAV. Concordance between immunofluorescence and antigen testing was highest in primary AAV (87.5%), followed by drug-induced AAV (42.9%), and IE-related GN (36.3%) (p< 0.001).
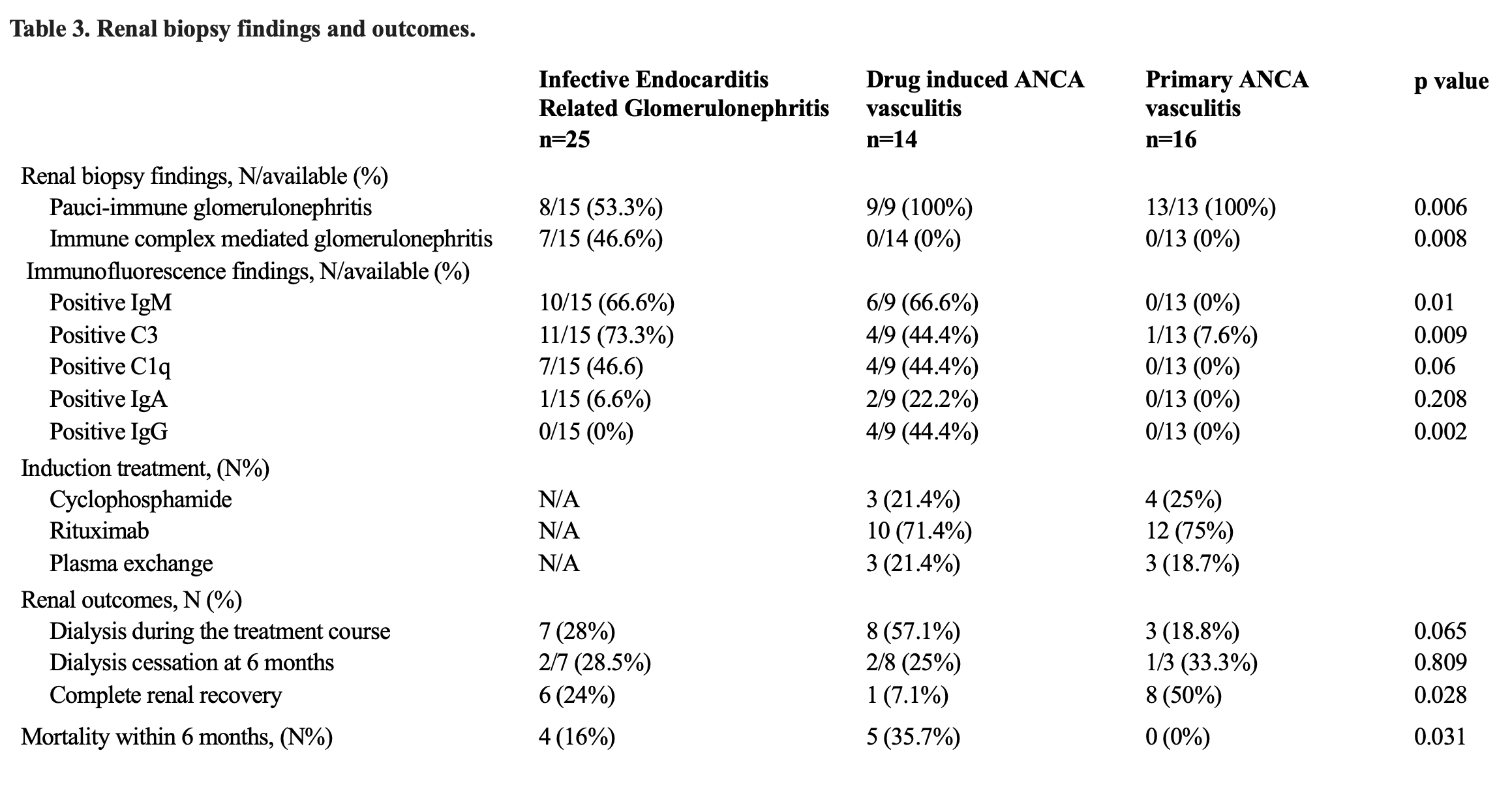
Majority of patients underwent renal biopsy (Table 3). IgM was the most common immunofluorescence finding in IE-related GN and drug-induced AAV (66.6%). Complete renal recovery occurred in 50% of primary AAV patients, 25% of IE related GN patients, and 7.1% of drug-induced AAV patients (p=0.028). Six-month mortality was significantly higher in IE related GN and drug induced AAV compared to primary AAV (p=0.031).
Conclusion: Secondary causes of ANCA positivity such as IE and drug induced AAV with GN are more likely to present with leukopenia, thrombocytopenia and low serum complements compared to primary AAV patients. This finding can help raise clinicians’ suspicion of a secondary process occurring when evaluating a patient with ANCA positivity. A prospective study with a larger sample size is required to validate the findings of this study.
To cite this abstract in AMA style:
Vural A, Yaseen K, Calabrese C, Brown A. Differentiating Primary Anti-Neutrophil Cytoplasmic Antibody (ANCA) Associated Vasculitis from Secondary Forms [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/differentiating-primary-anti-neutrophil-cytoplasmic-antibody-anca-associated-vasculitis-from-secondary-forms/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/differentiating-primary-anti-neutrophil-cytoplasmic-antibody-anca-associated-vasculitis-from-secondary-forms/