Session Information
Date: Saturday, November 16, 2024
Title: SpA Including PsA – Diagnosis, Manifestations, & Outcomes Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Axial spondyloarthritis (AxSpA) encompasses both non-radiographic axial spondyloarthritis (nr-AxSpA) and radiographic axial spondyloarthritis (r-AxSpA), also known as ankylosing spondylitis (AS). Although nr-AxSpA is often an early stage of AS, the differences between these entities are evident.
The objective is to evaluate the difference in prevalence of intestinal inflammation, defined as a diagnosis of inflammatory bowel disease (IBD) or elevated fecal calprotectin as a surrogate marker, between r-AxSpA and nr-AxSpA.
Methods: Data from patients with AxSpA from the EISER study (patients ≥18 years old treated at the Spanish National Health System Rheumatology Services, diagnosed according to ASAS criteria) were analyzed.
Patients attended a visit with a rheumatologist who collected demographic and clinical data (HLA27, disease activity, CRP, ESR) and treatment information. Subsequently, a fecal calprotectin (FC) test using the Quantum Blue rapid test was performed, and patients with an FC ≥80 μg/g underwent an endoscopic study. For patients with normal endoscopy results, a capsule endoscopy or magnetic resonance enterography was conducted.
Quantitative variables were described using median and interquartile range (IQR). Qualitative variables were described with absolute and relative frequencies. The Kruskal Wallis test was used to compare variables, considering significant if p< 0.05.
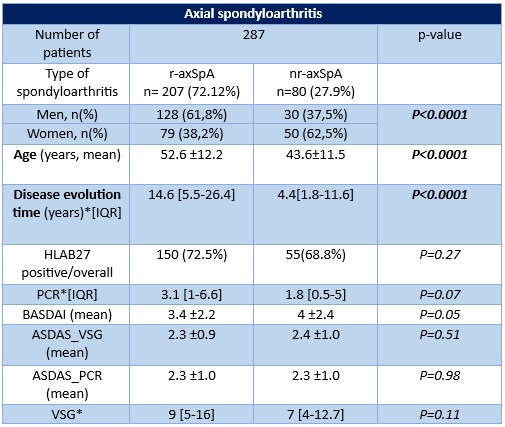
Results: A total of 287 patients with AxSpA were included, with patients with AS being more prevalent than nr-AxSpA (72.1% vs. 27.9%). Regarding sex distribution according to the type of AxSpA, clinically significant differences were found in both groups (p< 0.0001), with AS being more prevalent in men (61.8%) while nr-AxSpA was more prevalent in women (62.5%). The disease duration was significantly longer in patients with AS compared to those with nr-AxSpA (14.6 years vs. 4.4; p< 0.0001). There were no significant differences in CRP data between the types of AxSpA (3.1 vs. 1.8, p=0.07) or other clinical variables (Table 1).
The medians of CF levels in patients with r-AxSpA were significantly higher than in patients with nr-AxSpA: 73.0 μg/g (IQR: 30.7; 249.3) (n=198/207) vs. 41.0 μg/g (IQR: 30.0; 118.0), p < 0.013 (n=75/80), respectively. Considering only those patients with CF≥ 80 μg/g, the significance was maintained: 269.0 μg/g (IQR: 174.7; 554.8) (n=94/104) in the case of r-AxSpA vs. 192.0 μg/g (IQR: 134.0; 359.0) for nr-AxSpA, (n=23/75), p< 0.001. Among the patients with CF performed and endoscopic test done, the prevalence of IBD was significantly higher in patients with EA compared to patients with nr-AxSpA (n=20/179; 11.2% vs. n=2/69; 2.9%, p=0.04).
Conclusion: Intestinal inflammation is a frequent extra-musculoskeletal manifestation in AxSpA. The prevalence was much higher in AS than in nr-AxSpA, and the duration of the disease might be one of the variables involved in this difference.
To cite this abstract in AMA style:
Merino C, Plaza Z, Gratacos Masmitja J, Rodríguez-Lago I, Trujillo E, Marin-Jimenez I, Perez Pampin E, Barreiro M, Hernández-Hernández V, Carrillo-Palau M, Garcia Vivar M, Muñoz M, Ladehesa-Pineda M, Iglesias Flores E, González-Lama Y, Arevalo Salaet M, Calvet X, Gutierrez-Casbas A, SANZ SANZ J. Different Prevalence of Intestinal Inflammation in Radiographic and Non-radiographic Axial Spondyloarthritis. Data from EISER Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/different-prevalence-of-intestinal-inflammation-in-radiographic-and-non-radiographic-axial-spondyloarthritis-data-from-eiser-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/different-prevalence-of-intestinal-inflammation-in-radiographic-and-non-radiographic-axial-spondyloarthritis-data-from-eiser-study/