Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Current treatment of knee osteoarthritis (OA) is focused primarily around pain relief offering sustained mobility and prioritizing symptom relief over disease progression potentially impacts treatment outcome in the longer term for patients. With candidate therapies being investigated to address disease progression, it is important to examine if and where differences exist, with the prescribing behavior of current treaters of knee OA.
Methods: A cross-sectional chart review survey was conducted in Q2 2019 among US rheumatologists (rheums), orthopedic surgeons (orthos), primary care physicians with a focus in sports medicine (SM PCPs), and pain specialists practicing across hospital and private practices. Recruited from a large access panel, physicians were screened for duration of practice in their specialty (3-50 years) and caseload (35 or more knee OA patients, at least 10 of which must be classified as moderate-severe). Participants were asked to complete a 3-part survey: (1) a doctor demographic questionnaire, (2) a perceptual questionnaire, assessing perception of available and upcoming OA therapies, and (3) patient charts for the next 5 knee OA patients seen following receipt of the survey, capturing demographics and treatment history. Data were analyzed using descriptive statistics.
Results: A total of 275 physicians were recruited, reporting on 1375 patients in total (Table 1). When focusing primarily on patients with moderate-severe knee OA, this represented 65% of patients for SM PCPs and orthos. Pain specialists and rheums by comparison, had a significantly larger caseload of moderate-severe patients, at 79% and 77% respectively.
When looking at the proportion of patients treated with prescription medication for their knee OA, pain specialists and rheums stated an average of 69% and 68% of their managed patients, while SM PCPs stated 66%. Orthos stated a significantly lower proportion of patients treated with prescription therapy, at 55%.
Looking at therapies across specialties, orthos state greater use of traditional NSAIDs to treat their knee OA patients compared to pain specialists and SM PCPs (53% vs 36% vs 44%), with a significant difference to the stated use of rheums (35%). Rheums on the other hand, state significantly greater use of opioids compared to orthos, 18% vs 12% for mild opioids and 8% vs 1% for strong opioids.
From commonly used imaging techniques, X-ray and Magnetic resonance imaging (MRI) were used in greater proportion over ultrasound or computed tomography (CT) scan and when considering evidence of radiographic progression from imaging, rheums reported a significantly lower proportion of patients demonstrating radiographic evidence of bone erosion, compared to all specialties researched- 36% compared to 65% reported by orthos, 65% by SM PCPs and 75% by pain specialists.
Conclusion: From the sample surveyed, knee OA patients may exhibit differing outcomes based on the management adopted by their presiding clinician. With candidate therapies offering alternatives to how we currently treat knee OA, understanding nuances between treaters may prove an important consideration, when examining treatment outcomes in the longer term.
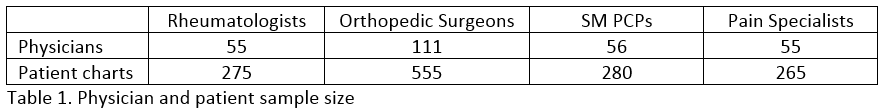 Table 1. Physician and patient sample size
Table 1. Physician and patient sample size
To cite this abstract in AMA style:
Baldock D, Zhang C. Differences in Treating Knee Osteoarthritis by Clinician Specialty [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/differences-in-treating-knee-osteoarthritis-by-clinician-specialty/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/differences-in-treating-knee-osteoarthritis-by-clinician-specialty/
