Session Information
Session Type: Abstract Session
Session Time: 3:30PM-3:45PM
Background/Purpose: The difference in spinal structural lesions and their progression over time between chronic back pain (CBP) patients with and without early axSpA is unknown. We aimed to compare structural lesions of the spine on conventional radiographs (CR) and magnetic resonance imaging (MRI) over 2 years (2Y), as well as their 2Y-change, between patients with early axSpA and non-axSpA CBP.
Methods: Patients included in the Spondyloarthritis Caught Early cohort (CBP ≥3 months and ≤2 years, starting < 45 years), were diagnosed with axSpA or non-axSpA CBP by their rheumatologist at 2Y follow-up (1). Only patients with available imaging (CR or MRI) at both baseline (BL) and 2Y were included. Spinal lesions on CR were assessed by three central readers using the modified Stoke Ankylosing Spondylitis Spine Score (mSASSS). Structural lesions on spinal MRIs were assessed by two central readers using the Canada-Denmark scoring system. Readers made assessments independently, and they were blinded to demographic, clinical data and to the chronological order. BL spinal structural lesions and 2Y changes were compared between axSpA and non-axSpA. Generalized Estimating Equations models were used to assess the progression of structural lesions over 2Y, adjusting for age, sex, NSAID use, and diagnosis.
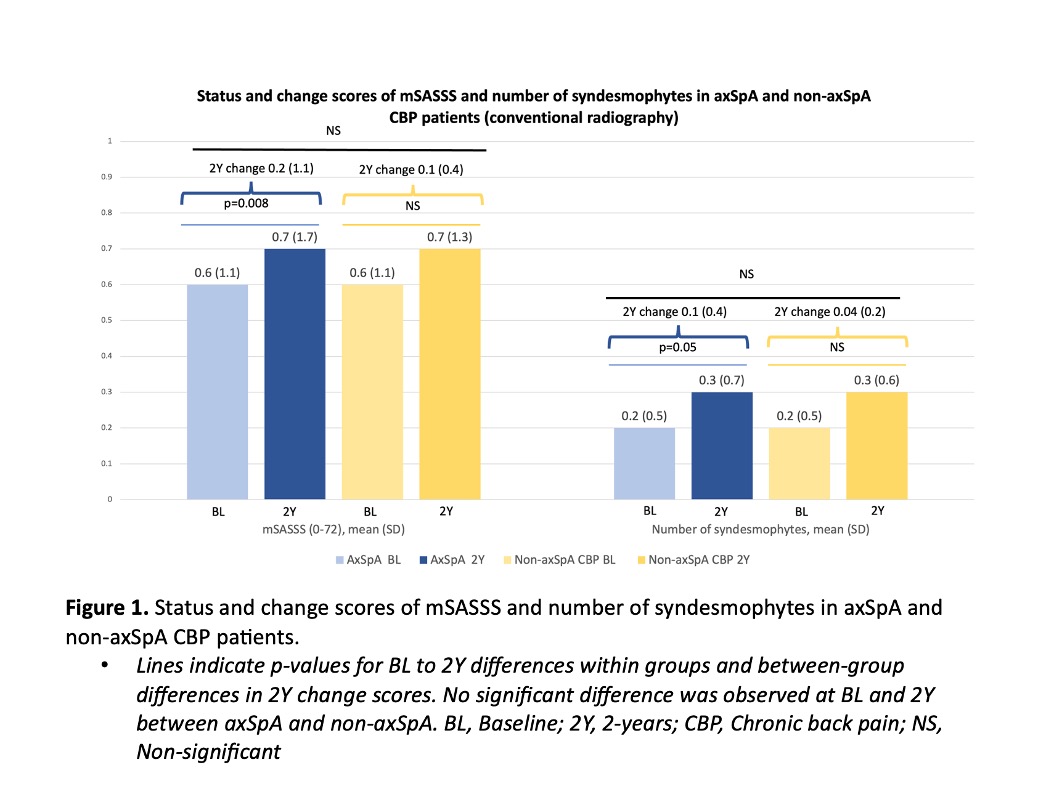
Results: CR data from 318 patients (67% axSpA) and MRI data from 351 patients (69% axSpA) were included. Overall, 278 patients had both CR and MRI available at BL and 2Y [mean (SD) age 30 (8) years, 46% males, 61% HLA-B27+]. On CR, the mean (SD) BL mSASSS was 0.6 (1.1) for both axSpA and non-axSpA (Figure 1). Over 2Y, the progression of spinal structural lesions was similar between the axSpA and non-axSpA groups on CR, with overall mSASSS progression being minimal, specifically 0.01 mSASSS units per year. Mean number of syndesmophytes at BL and 2Y change scores between patients with axSpA and non-axSpA were similar. On MRI, axSpA patients had a mean of 1.4 (2.9) total structural lesions compared to 0.7 (2) in non-axSpA at BL (p=0.12) (Figure 2A). The 2Y increase in the mean total number of structural lesions [0.5 (1.8)] was mainly driven by the increase in fat lesions [0.5 (1.6)] in the axSpA group and was significantly higher than in non-axSpA (Figure 2B). The proportion of patients with ≥3 fat lesions both at BL and 2Y was higher in the axSpA group (BL: 9% vs 1%, p=0.004, 2Y: 15% vs 1%, p< 0.001). On MRI, fat lesions progressed at a rate of 0.16 units/year in axSpA (p=0.002) and -0.02 units/year in non-axSpA (p=0.7). The remaining lesions showed no significant progression.
Conclusion: Over 2 years, there is minimal progression of spinal structural damage typical for axSpA on CR in both early axSpA and non-axSpA CBP. On MRI, there is a significant increase in the number of fat lesions in axSpA, contrasting with non-axSpA in which no progression is observed. Fat lesions may be important to assess spinal disease progression from early disease onwards.References: (1) Marques et al. Ann Rheum Dis. 2024;83(5):589-598
To cite this abstract in AMA style:
Ayan G, de Bruin L, van Lunteren M, de Hooge M, Bento da Silva A, Marques M, Reijnierse M, Navarro-Compan V, van de sande M, Jorid Berg I, Ramonda R, Exarchou S, Van Der Heijde D, van Gaalen F, Ramiro S. Differences in structural lesions of the spine between patients with early axSpA and non-axSpA chronic back pain: 2-year results of the SPACE Cohort [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/differences-in-structural-lesions-of-the-spine-between-patients-with-early-axspa-and-non-axspa-chronic-back-pain-2-year-results-of-the-space-cohort/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/differences-in-structural-lesions-of-the-spine-between-patients-with-early-axspa-and-non-axspa-chronic-back-pain-2-year-results-of-the-space-cohort/

.jpg)