Session Information
Session Type: Abstract Session
Session Time: 1:15PM-1:30PM
Background/Purpose: Individuals with systemic autoimmune rheumatic diseases (SARDs) are at risk for worse acute and post-acute COVID-19 outcomes due to use of immunosuppressive medications and possibly prolonged viral shedding. Whether individuals with SARDs have higher levels of viral antigens and/or longer persistence of viral antigens after COVID-19 has not been studied.
Methods: We evaluated differences between an immunocompromised state and prolonged SARS-CoV-2 antigen (spike, S1 [Spike protein that contains the receptor binding domain], and nucleocapsid) positivity after COVID-19 in two prospective cohorts. We studied immunosuppressed individuals with SARDs in the RheumCARD study at a large US healthcare system and immunocompetent individuals in the RECOVER study. SARS-CoV-2 antigens were measured in collected plasma or serum samples using previously validated ultra-sensitive single molecule array, a digital enzyme-linked immunosorbent assay that uses antibody-coated magnetic beads to capture antigen molecules, which are then detected and loaded into microwell arrays through the enzymatic cleavage of a fluorescent substrate. We used logistic regression to evaluate unadjusted and adjusted (for age, sex, calendar year of infection, and vaccination status at the time of infection) odds ratios for SARS-CoV-2 antigen positivity comparing RheumCARD vs. RECOVER at 3 and 6-months following COVID-19.
Results: Among 210 immunocompromised individuals with SARDs in RheumCARD and 429 immunocompetent individuals in RECOVER (Table), the mean age was 56.3 vs. 45.0 years, respectively, and 81.0% vs. 66.4% were female in each cohort. COVID-19 occurred in pre-Omicron variants (before 12/16/2021) in 37.6% of RheumCARD vs. 33.8% of RECOVER. Most individuals were vaccinated at the time of infection (73.3% in RheumCARD vs. 89.0% in RECOVER). Among those with SARDs, the most common SARD type was inflammatory arthritis (61.0%) and most (53.8%) had low disease activity. Many patients (31.4%) were receiving conventional synthetic DMARDs only, with 25.2% receiving TNF inhibitors and 8.6% receiving CD20 inhibitors. A minority (15.7%) were receiving glucocorticoids at the time of infection. At the time of blood draw, any SARS-CoV-2 antigen positivity was more common in those with SARDs (36.7% in RheumCARD vs. 18.9% in RECOVER; p< 0.001) (Figure 1). Those with SARDs had higher odds of nucleocapsid antigen positivity (adjusted OR 3.17, 95%CI 1.21-8.33) or any antigen positivity (adjusted OR 2.68, 95%CI 1.38-5.20) 3 months after COVID-19 (Figure 2). At 6 months following COVID-19 infection, nucleocapsid antigen positivity remained significantly higher among those with SARDs (adjusted OR 6.92, 95%CI 1.21-39.43).
Conclusion: Individuals with SARDs were more likely to have SARS-CoV-2 antigen positivity at 3 and 6 months following COVID-19 infection compared with immunocompetent individuals, not explained by demographics, variant, or vaccination. Persistent nucleocapsid antigen positivity, a marker of viral shedding rather than vaccination, was the greatest driver of differences between groups, suggesting that an immunocompromised state may result in prolonged antigenemia.
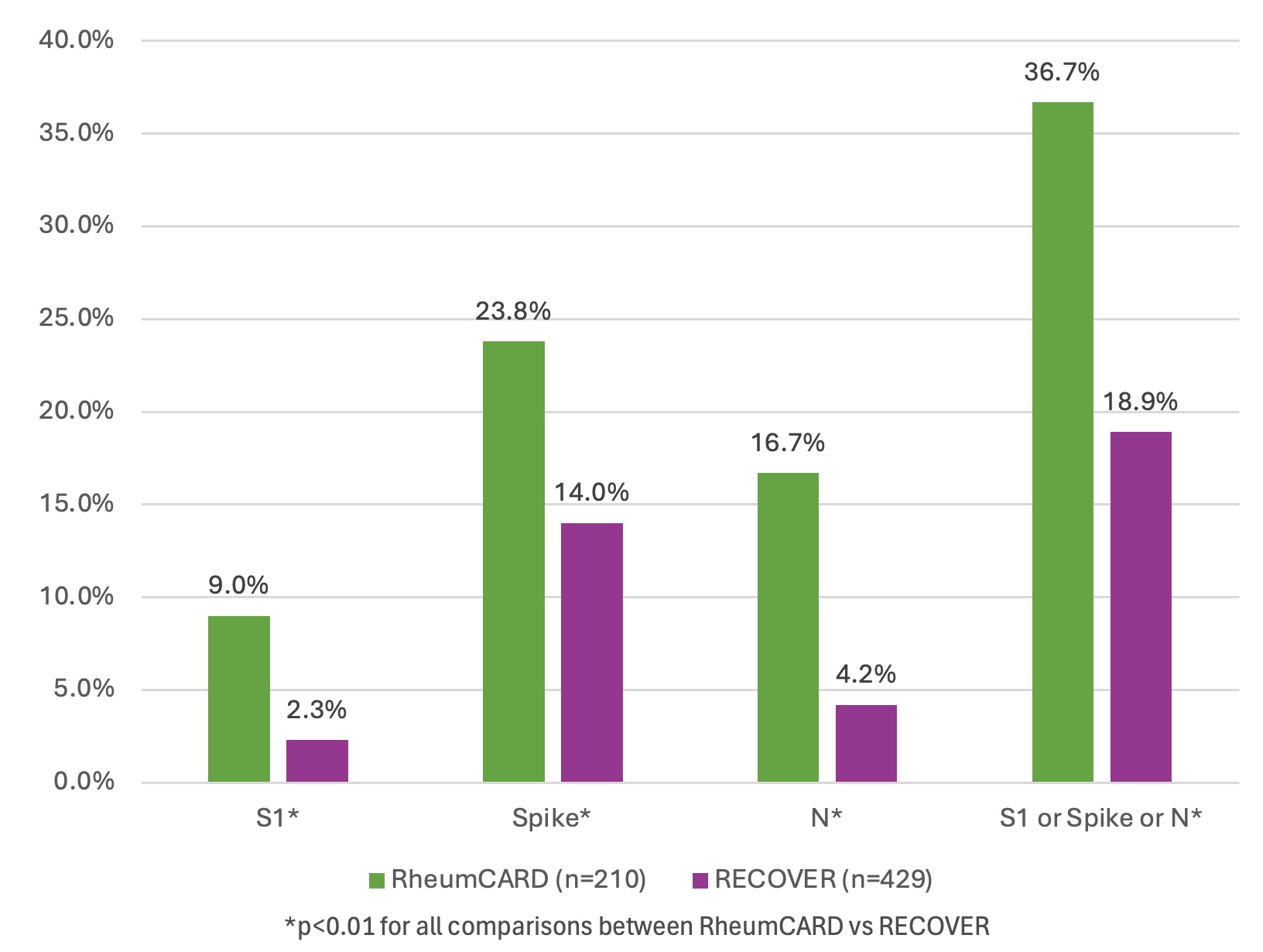 Table. Baseline characteristics at the time of sample collection for post COVID-19 cases in the RheumCARD and RECOVER cohorts
Table. Baseline characteristics at the time of sample collection for post COVID-19 cases in the RheumCARD and RECOVER cohorts
.jpg) Figure 1. Frequency of positive SARS-CoV-2 antigens (S1 [spike protein that contains the receptor binding domain], spike, or nucleocapsid [N]) after COVID-19 in the RheumCARD vs. RECOVER cohorts at time of blood draw
Figure 1. Frequency of positive SARS-CoV-2 antigens (S1 [spike protein that contains the receptor binding domain], spike, or nucleocapsid [N]) after COVID-19 in the RheumCARD vs. RECOVER cohorts at time of blood draw
.jpg) Figure 2. Differences in antigen positivity in the RheumCARD vs. RECOVER cohorts at 3 and 6 months following COVID-19 infection
Figure 2. Differences in antigen positivity in the RheumCARD vs. RECOVER cohorts at 3 and 6 months following COVID-19 infection
To cite this abstract in AMA style:
Patel N, Swank Z, Wang J, Wang X, O'Keeffe L, Negron M, Getachew L, Hansen L, Qian G, Saavedra A, Mueller K, Davis N, Vanni K, Wallace Z, Walt D, Sparks J. Differences in SARS-CoV-2 Antigen Persistence in Individuals with Systemic Autoimmune Rheumatic Diseases Compared to the General Population [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/differences-in-sars-cov-2-antigen-persistence-in-individuals-with-systemic-autoimmune-rheumatic-diseases-compared-to-the-general-population/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/differences-in-sars-cov-2-antigen-persistence-in-individuals-with-systemic-autoimmune-rheumatic-diseases-compared-to-the-general-population/
